
iStock #859186988
In the wake of the barefoot running trend, a blurry distinction has been made between barefoot running/exercise and barefoot training. A training protocol needs to be defined based on current research and proven therapeutic exercise standards.
By William Smith, MSPT, C.Ped.
On January 17, 2011, The New York Times published an article titled “Close Look at Orthotics Raises a Welter of Doubts.”1 Responding to the writing and research of Benno Nigg,2 it called into question much of the anecdotal information we provide to our patients when prescribing footwear and foot orthotics. The article questioned the biomechanical efficacy of specific footwear and foot orthoses as it relates to performance enhancement, injury treatment, and injury prevention.1 The article prompted me—and many other clinicians—to reassess my treatment rationales. Upon reading Nigg’s book, Biomechanics of Sports Shoes2 in its entirety, I found myself trying to justify the treatment strategies I had developed and questioning my rationale for providing them. In many cases, I would look at a patient who had responded well to a combination of physical therapy, the use of custom foot orthotics, and a home exercise and training program. I felt like my treatments were working, but it may not have been for the reasons I had thought.
One thing I found illuminating in Nigg’s book—which was not mentioned in The New York Times article—is the concept of barefoot training. Nigg refers to barefoot training as a focal point of research and development in the “improvement of human locomotion” and as a “future direction” for the biomechanical research of footwear and performance.2 I have always embraced this concept when working with my patients, and I believe barefoot training can be embraced by both sides of the barefoot/minimalist shoe debate once a clear distinction and protocol is defined.
What the Times article did not question is the significant role the muscles of the foot play in foot structure and function. This idea can be incorporated into any foot care practice without the need for patients to abandon their shoes and foot orthotics.
Exercise vs Training
Exercise is physical activity done for its own sake. Training is physical activity performed for the purpose of satisfying a long-term performance goal. Training describes the process rather than the workouts themselves.
When performing an initial patient evaluation, I will often ask, What is it that you love to do? Regardless of the patient’s response, be it hiking, dancing, running a marathon, or playing basketball, I always tell them the same thing: We train to keep doing what we love. Doing what you love is not training. Barefoot training merely refers to training the muscles that cross the foot and ankle joint in pursuit of a specific goal, which may be recovering from an injury, returning to a sport, or preventing future problems before they arise. It is not mutually exclusive to barefoot or minimalist shoe wearers. Anyone can benefit from a foot and ankle strengthening program.
Training Principles
Triplanar Training Program Components
Closed chain vs. open chain: Functional progress from open chain, non-resisted training to resisted non-weight bearing triplanar exercises should be completed before advancing to dynamic weight-bearing activities.
Eccentric vs concentric: The forefoot musculature is eccentrically loaded during landing and resists transverse shearing forces. Eccentric control is vital to the pretibial and longer sagittal plane musculature; therefore, a combination of concentric and eccentric training is imperative.
Proprioceptive training: The loss of proprioception and sensation—in the neuropathic foot, for example—is devastating. Therefore, proprioceptive training should be incorporated into any comprehensive training regimen.
Indirect experimental evidence for the importance of training the small muscles was provided in a study that quantified the frequency of injury in adolescents with and without wobble-board training.4,6 The study found that the participants exposed to wobble-board training had fewer sport-related injuries than those who were not exposed to this training. It was speculated that wobble-board training strengthened the small and large muscles and provided more all-around development, especially for muscles crossing the ankle joint where many small muscles may be involved in motion and motion control.4,6 Wobble-board training and barefoot training both strengthen the small and large muscles crossing the ankle joint (Figure 4).

Figure 4: Exercise device for proprioceptive training in standing with miniature wobble board integrated with forefoot bed. During wobble board exercises, proprioceptive information is generated by ligamentous mechanoreceptors, Golgi tendon organs, and muscle spindles, which transduce mechanical distortion of the surrounding connective tissue. Stability of the ankle joint during functional activities depends on the presence of intact neural input from proprioceptors in the joint capsules, ligaments, muscles, tendons, and skin.
Specificity
As with any training regimen, we have to identify which muscle we are training, in which plane of motion we are working, and how the muscles being trained work during a functional activity. We need to know whether a muscle group works eccentrically, concentrically, or isotonically, as well as whether the movements are in a closed or open chain. It is important to differentiate between the intrinsic and extrinsic muscles of the foot. The intrinsic muscles of the foot act as isotonic stabilizers to transverse plane forces. When training the extrinsic foot muscles, an important distinction must be made between the long extrinsic muscles and the short extrinsic muscle that cross the ankle joint (Figure 1). Nigg discusses how “larger muscles may have lines of action that are not optimal for sensing changes in specific directions.”2 In the ankle joint complex, the triceps surae and tibialis anterior are ideal for sensing changes in flexion/extension movement (dorsiflexion and plantar flexion), but they are not well suited for sensing changes in foot abduction/adduction and inversion/eversion. For many changes in position, there are small muscles that can provide joint stability quickly and with little force, and although one does not voluntarily select specific muscles to stabilize a joint, training these small, quick muscles increases the general stability of the ankle joint. This concept is universal to all joints in the body and can best be seen in the shoulder joint complex, which requires the training of the small rotator cuff musculature to facilitate joint stability prior to progressing to more functional movements such as throwing a ball or lifting an object.
Progression
Many articles and blogs on barefoot running use the term transition when discussing beginning a barefoot running program. Writers typically advise people to begin running barefoot gradually and increase the distance as tolerated.3,4 This concerns me as a physical therapist who helps many people return to or begin a new activity after an injury. That advice is similar to telling a shoulder patient to start throwing the ball a little bit each day and gradually transition to pitching fastballs. As with any exercise routine, a progression from open-chain, single-plane, non-weight bearing exercises needs to be initiated before progressing to resisted closed-chain exercises. Triplanar-resisted, closed-chain activity is performed semi-weight- bearing before full weight-bearing activities. Finally, training should gradually progress to dynamic/plyometric activities before running or participating in a new sport (Figure 2).
Overload
To increase strength and endurance, you need to increase resistance, time, or intensity in your training efforts. This principle works in concert with progression. To run a 10-kilometer race, athletes need to build up distance over repeated sessions in a reasonable manner to improve muscle adaptation and improve soft-tissue strength and resiliency. Any demanding exercise attempted too soon risks injury. The same principle holds true for strength and power exercises. A study comparing runners transitioning to Vibram FiveFingers™ minimalist shoes to a control group of runners using traditional running shoes showed a correlation between intrinsic foot muscle size and injury prevention in individuals in the minimalist shoe transition group.5 The authors hypothesized that intrinsic foot muscle strengthening would benefit runners who want to transition to minimalist shoes.
Adaptation
Over time, the body becomes accustomed to exercising at a given level. This adaptation results in improved efficiency, less effort, and less muscle breakdown at that level. That is why people experience muscle soreness when they run two miles for the first time, but it becomes a warm-up for the main workout after regular practice. This is also why it is necessary to run at a higher intensity or for a longer duration to continue improving. The same holds true for adapting to lesser amounts of exercise. One specific exercise or activity cannot be relied upon to maintain strength and flexibility. A training regimen should challenge the body through a complete range of motion in all planes of motion. Training programs for the foot and ankle are no exception.
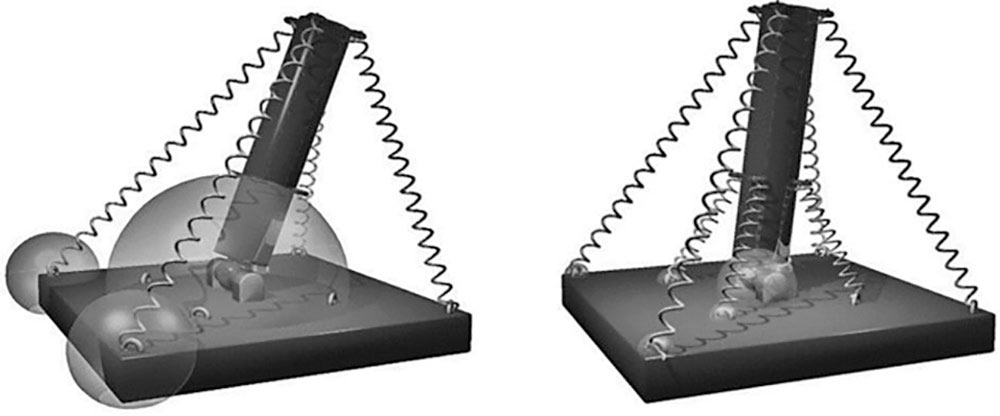
Figure 1: Effect of strong and weak small springs (muscles) on forces in the joint and in the attachment locations of the springs (insertion forces). The simulations were made assuming that the small springs react faster than the large springs.2 (Used with permission.)
Planes of Motion
Nigg and others have pointed out the importance of training a triplanar joint in three planes of motion.2,3,4,6 When looking at the progressively shorter muscles of the lower leg and foot, the longer muscle such as tibialis anterior and triceps surae can be viewed as primary sagittal movers. The shorter, deep extrinsic muscles that originate closer to the ankle joint they cross have more stability in the frontal and transverse planes. The intrinsic foot muscles help to control transverse plane motions. When assessing planes of motion, it is imperative to assess for and address any sagittal plane limitations early on in the training regime. An assessment of ankle dorsiflexion and first metatarsophalangeal extension is an integral part of the initial assessment. Any limitation in sagittal motion at the foot and ankle will lead to subsequent compensation in the frontal and transverse planes (Figure 3).
I attended a lower extremity functional sports-specific training course early in my career. The instructor made a statement that stays with me to this day: “The majority of lower extremity injuries and pathologies occur in the transverse plane; therefore, we must train in the transverse plan.”
There are not many studies that examine resistive training when dealing with transverse plane mechanics, but one study of note examined the use of orthoses and resistive exercise for the treatment of posterior tibial tendon dysfunction.7 Participants were randomly assigned to one of three groups to complete a 12-week program: 1) orthoses wear and stretching (O group); 2) orthoses wear, stretching, and concentric progressive resistive exercise (OC group); or 3) orthoses wear, stretching, and eccentric progressive resistive exercise (OE group). Pre-intervention and post-intervention data (Foot Functional Index, distance traveled in the 5-minute walk test [5MWT], and pain immediately after the 5MWT) were collected.7
Foot Functional Index scores (total, pain, and disability) decreased in all groups after the intervention and pain immediately after the 5MWT was significantly reduced across all groups as well.7 Notably, the OE group demonstrated the most improvement in each subcategory, and the O group demonstrated the least improvement.
Muscle Tuning
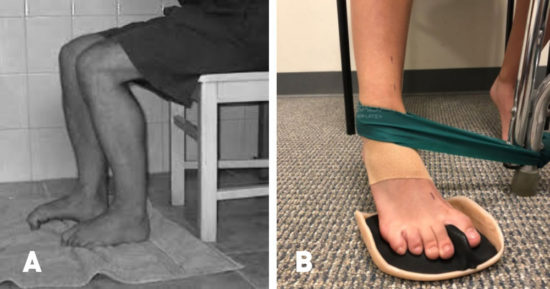
Figure 2: (A) A common exercise given by physical therapists is the classic toe curl exercise. Although this exercise is beneficial for improving general range of motion and helping to activate the toe flexors following an injury, it is not a functional movement. (B) I prefer sagittal plane concentric toe flexion progressed to resisted, triplanar motion with eccentric stabilization in the transverse plane.
Nigg hypothesized that we tune our muscular response to ground impact from step to step in order to minimize vibrations that pass through the soft tissues of our lower limbs.2,8-10 Based on this theory, the intrinsic muscles of the foot can be thought of as having two distinct roles:
- Stabilizing the forefoot in the transverse plane as sagittal plane forces are transmitted through the foot in preparation for terminal stance.
- “Tuning” or pre-activating for landing on initial contact. This is a proprioceptive neuromuscular concept that allows the foot to adapt to varying surfaces. Nigg described a case in which a Cirque de Soleil group suffered performance-stopping injuries at a rate of 25%. Upon examination, it was determined that the stage was constructed in such a way that surface hardness varied throughout the stage. Once the stage was reinforced and made uniformly hard, injury rates dropped to 2%-3%.
Foot Orthotics and Foot Musculature
Some of my most successful treatments have involved the use of custom-fabricated foot orthotics. Could the reason for their success be related to how a foot orthotic affects the function of the intrinsic foot musculature during the stabilizing and turning processes? Does a custom foot orthotic provide a uniform surface for the foot to “pre-activate” to?
When designing foot orthotics for athletes, I often stress the need for forefoot stabilization and a total-contact, molded interface with the toes. Does this provide an ergonomic interface for the forefoot to stabilize the hindfoot as sagittal plane forces are transmitted to transverse plane at terminal stance?
These questions are contrary to the traditional Root-based biomechanics upon which foot orthotic professionals have been raised. Does the stabilization of the hindfoot elicit forefoot stability, or could it be the other way around if muscle tuning is responsible for pre-activation at forefoot landing in runners? Is it possible that both of these processes occur simultaneously?
As a physical therapist, pedorthist, and inventor, I am constantly trying to provide comprehensive solutions for biomechanical problems. Many patients simply want to do what they love as long as they can without pain.

Figure 3: Exercise device (Tib Post Loader) designed to provide progressive, constant resistance (0.9–9 kg) in the transverse plane. The hand lever (3) allows for selective application of resistance in one direction only. When the footplate is moved by the foot against the resistance of the spring (2) into horizontal adduction, the tibialis posterior tendon is recruited concentrically. Conversely, when the foot resists the motion of the footplate toward horizontal abduction, the tibialis posterior tendon is recruited eccentrically. To minimize the activity of the anterior tibialis tendon with transverse plane motion, secondary static resistance (0.9 kg) to plantar flexion is provided. Light-emitting diodes indicate whether the foot is pressing into plantar flexion.
When I talk with other therapists about pedorthics in general and the use of foot orthotics in particular, the most common reason for not utilizing foot orthotics is the fear of weakening the foot. Much of the training I and many other physical therapists received in school is based on the theory of stopping or preventing pathological movement of the foot by designing a subtalar neutral foot orthotic that maintains the foot in an “ideal” biomechanical position. As a result, many physical therapists are reluctant to recommend foot orthotics to their patients for fear of stopping the movement that is essential for the foot during activity. However, new research and theories are emerging in biomechanics that challenge the mechanisms through which foot orthotics work. Recent articles have described foot orthotics as more of a proprioceptive feedback tool.3,11,12 Our feet are highly innervated structures that must constantly respond to feedback from the ground for us to maintain our center of gravity over our feet during locomotion. A recent study of 21 healthy runners utilizing various foot orthotics revealed small but significant kinematic changes of around 2 degrees, but in most of the cases, muscle activity increased with the foot orthotics.3
Conclusion
The key component of any training program is the initial assessment of active, passive, and neural structures that provide dynamic foot control during activity.11,12 In order to quantifiably correlate foot and ankle strength with injury prevention and performance, more consistent foot and ankle strength measurement parameters are needed. Isokinetic testing in three planes of foot and ankle motion may provide usable data going forward. Proprioceptive measurement tools need to be developed that will not only assess strength but will also assess reaction time and joint kinematics. The term muscle imbalance is often used by clinicians in treating biomechanics. As tools are developed that can quantitatively measure muscle strength specifically in the transverse plane, a more definitive connection may be revealed. This may pave the way for universally accepted barefoot training protocols in a field that is often divided regarding the management of foot and ankle function.
William Smith is the owner of In-Step Physical Therapy in Albany, NY, and has been practicing as a physical therapist and certified pedorthist for over 17 years. For more information visit www.insteppt.org.
- Kolata G. Close look at orthotics raises a welter of doubts. New York Times. Jan. 17, 2011; page 5.
- Nigg BM. 2010. Biomechanics of sport shoes, 1st ed, Calgary: Topline Printing.
- Chen TL, Sze LK, Davis IS, Cheung RT. Effects of training in minimalist shoes on the intrinsic and extrinsic foot muscle volume. Clin Biomech (Bristol, Avon). 2016;36:8-13.
- Emery CA, Cassidy JD, Klassen TP, et al. Effectiveness of a home-based balance-training program in reducing sports-related injuries among healthy adolescents: a cluster randomized controlled trial. CMAJ. 2005;172(6):749-54.
- Johnson AW, Myrer JW, Mitchell UH, Hunter I, Ridge ST. The effects of a transition to minimalist shoe running on intrinsic foot muscle size. Int J Sports Med. 2016 Feb;37(2):154-8. doi: 10.1055/s-0035-1559685. Epub 2015 Oct 28.
- Karakaya MG, Rutbİl H, Akpinar E, Yildirim A, Karakaya IC. Effect of ankle proprioceptive training on static body balance. J Phys Ther Sci. 2015; 27(10): 3299–3302.
- Kulig K, Reischl SF, Pomrantz AB, et al. Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: a randomized controlled trial. Phys Ther. 2009;89(1):26-37.
- Wakeling JM, Nigg BM. Modification of soft tissue vibrations in the leg by muscular activity. J App Phys. 2001;90(2): 412–420.
- Wakeling JM, Nigg BM. Soft-tissue vibrations in the quadriceps measured with skin mounted transducers. J Biomech. 2001;34(4): 539–543.
- Wakeling JM. Muscle activity in the leg is tuned in response to ground reaction forces. J App Phys. 2001;91(3): 1307–1317.
- McKeon PO, Fourchet F. Freeing the foot: integrating the foot core system into rehabilitation for lower extremity injuries. Clin Sports Med. 2015;34(2):347-61.
- McKeon PO, Hertel J, Bramble D, Davis I. The foot core system: a new paradigm for understanding intrinsic foot muscle function. Br J Sports Med. 2015;49(5):290.









