Evidence suggests that foot orthoses can help relieve painful knee symptoms and possibly even help prevent injury. The key may be pronation control, which in turn affects tibial internal rotation and frontal plane alignment.
The medical literature was silent about the mechanical origins of knee pain until, in my opinion, the athletic medical community recognized a possible causal relationship between hypermobile foot joints and knee pain in runners. Knee pain had previously been considered the result of osteoarthritis and was thought to have no other etiology except ligamentous damage resulting in unstable knee joints. The effect of foot motion was not a consideration. Now, however, the literature reflects a more complete understanding of the pathomechanics of mechanically induced knee pain and the role of foot orthoses in treatment.
Not all knee pain should be attributed to abnormal mechanics. Similarly, intervention with biomechanics-altering devices to treat all knee pain regardless of origin will surely result in more treatment failures than successes. The literature suggests that the origin of most knee pain is mechanical, especially in the athlete. But mention must be made of the other potential causes of knee pain before one can establish a theoretical foundation for the use of foot orthoses. Ruling out the other differential diagnoses is essential for successful orthotic therapy. Anecdotally, the imitators include damage to intra-articular structures (particularly the menisci and their coronary ligaments), collateral ligament damage, peripatellar tendinitis or bursitis, plica syndromes, Osgood-Schlatter’s disease, neuromas, ganglions and several other but rarely occurring pathologies.
The mechanical origins of a patient’s knee pain can often be brought to light by attempting to alter the mechanics of the lower extremity to see if symptoms improve. Strapping, taping, hamstring-strengthening exercises, wedge padding and prefabricated orthoses offer inexpensive diagnostic tools to ascertain that the symptoms also are mechanical in origin (with the understanding that, as with other diagnostic tools, false negative results are possible). 1-4
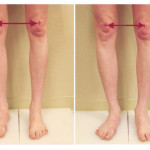
Figure 1. Pronation of the subtalar joint with subsequent collapse of the midtarsal joint creates internal rotation of the tibia and produces a significant rotational torque on the knee. Orthotic control of the foot limits both the amount and velocity of the internal rotation.
Knee pain pathology, for the purpose of this article, can be divided into three anatomical or geographic areas: anterior knee pain, referred to most recently as patellofemoral pain syndrome (PFPS); medial or lateral knee pain; and ligamentous knee injuries, primarily injuries of the anterior cruciate ligament, which appear more frequently in female athletes.
Targeting the tibia
The amount of tibial internal rotation and the resulting transverse plane moment at the knee joint is determined by pronation of the subtalar joint and consequential collapse of the midtarsal joint.5,6 It has been further suggested that the amount and velocity of excessive foot pronation increases the amount and force of tibial internal rotation.7 This process increases the dislocation moment at the knee in the transverse plane. Demonstrations have shown that joint forces and particularly moments at the knee joint can be altered using orthoses during running.8
The frontal plane biomechanics that lead to medial and lateral knee pain were once thought to be controlled proximally by the position of the femur at the hip joint, altering the position of the knee in either genu valgum or varum. Reducing the Q angle in patients with genu varum at single limb support increases the inversion moment on the knee joint.9 Published data suggest that lateral wedging of various foot orthotic designs can reduce this inversion moment at the knee joint, an important function of foot orthoses.9
The etiology of PFPS is believed to be multifactorial, but research suggests that the pathomechanics described above play a role.10 Specifically, studies linking foot posture to patellofemoral joint alignment suggests that Q angle is affected by tibial internal rotation as well as femoral anteversion.
One of the first kinematic running studies postulated that the transverse plane motion of the leg and the excessive frontal plane motion of the foot, in the direction of pronation, produce an abnormal coupling and contribute to malalignment of the patella upon the femur.5 An earlier study suggested that the excessive pronation and resulting internal tibial rotation of the leg produces a delay in external tibial rotation while the femur continues with an external rotation course, again creating a damaging torque on the knee.7,11 The relationship between Q angle and PFPS pain continues to be debated but a 1986 study did demonstrate a reduction in the Q angle when internal rotation is prevented by orthoses.12 This investigation demonstrated a causal relationship between the increased Q angle and PFPS and suggested that a potential solution may be at hand with custom functional orthoses.12-14
Orthotic outcomes

Figure 2. The lateral heel skive technique changes the symmetry of the heel cup, producing greater ground reaction force lateral to the subtalar joint axis.
Until methods are developed that confirm the exact link between abnormal foot mechanics and patellofemoral joint mechanics, clinicians will need to rely on outcome studies to guide their clinical decision making regarding orthoses, custom or otherwise. A number of studies overwhelmingly demonstrate a positive outcome using functional orthoses. Although the actual device used varies greatly with materials, construction, casting or flexibility, all are designed to limit foot motion between heel contact and heel lift, if not specifically to limit pronation of the subtalar joint.
Eng et al used soft foot orthoses with stretching/strengthening exercises for eight weeks in adolescent female patients with patellofemoral pain, and reported significantly greater reductions in pain during running and stair walking than a control group who only did the exercises.4 Another study used a semi-rigid thermoplastic device, in only one athlete, but found significant improvement in pain and function.15 Further, a study using custom semi-rigid orthoses in participants with patellofemoral pain found that ratings of stiffness, pain and physical function improved after using the devices for only two weeks.16 Also, a study that used classic custom functional devices intended to be Root type orthoses, fabricated from corrected and balanced positives, reported a 67% improvement in pain after six months. All but three out of 41 patients who completed follow-up questionnaires said they still wore their devices six months after initiating treatment.17 Interestingly, no reports suggest an increase in patellofemoral pain from the use of prefabricated or custom orthoses designed to slow, reduce or limit foot pronation.
Saxena’s 2003 article18 on PFPS captured the attention of the podiatric as well as the orthopedic and physical therapy communities. This retrospective review evaluated the effectiveness of custom semi-rigid Root type orthoses in 102 patients complaining of symptoms of either chondromalacia patellae, PFPS or retropatellar dysplasia. All subjects received similar functional custom devices, fabricated from neutral suspension casts and formed from polypropylene with rearfoot or forefoot posts. The majority of the rearfoot posts were 2º or slightly more in varus, a similar orthotic component to a 2 mm medial skive. Two to four weeks after orthosis dispensal, 76.5% of the patients reported improvement in knee pain with orthotic intervention. Two percent of the patients were asymptomatic and 17% had no change.
The most recent randomized clinical trial related to orthotics and knee pain evaluated the use of functional orthoses in the treatment of patellofemoral pain.14 The study compared a prefabricated functional orthotic therapy to treatment with a specific physical therapy protocol in an effort to reduce symptoms of PFPS. The prefabricated orthoses were designed to limit subtalar pronation.(Figure 1) Patients were randomized to receive the test orthoses, sham orthoses, physical therapy, or a combination of both physical therapy and orthoses.
Unfortunately, the test orthoses used were not just prefabricated; they were used not to control foot function but rather were “fitted to their shoes with comfort as a primary goal.” The test orthoses were also customized to some degree to “optimize comfort” through heat molding and by adding wedges or heel raises.
Regardless, the results of the study were still very impressive in terms of demonstrating the value of the orthoses. At six and 12 weeks, the test foot orthoses were significantly more effective than the sham devices for improvement in pain and function, and did as well as six 20 to 60 minute sessions of physical therapy, taping and home exercises combined. Combining physical therapy with orthotic therapy did not improve the outcome.
Most interesting is the treatment cost factor. The study was performed in Australia, where the physical therapy costs for the six sessions was $495. Three pairs of orthoses for each patient cost $174, including an estimate of consultation fees.
Medial compartment mechanics
Medial compartment knee pain pathomechanics present a totally different scenario than the mechanism that produces anterior knee pain. Medial knee pain primarily involves traction to knee ligaments and subsequent soft tissue injury, progressing to cartilaginous and osseous changes. Three articles identify a close association between excessive pronation of the foot and ACL injury.18-21 It has been well documented that pronation of the subtalar joint combined with the resulting midtarsal collapse produces excessive tibial internal rotation, causing the knee to move into valgus, which in turn increases tension on the ACL.22 Tension is also increased on the medial collateral ligaments when the knee is in a valgus position. Increased tension on the ligament of a joint usually results from forces that do not act perpendicular to the axis of the joint. These same dynamic forces can also induce the wear and tear on a joint that can lead to non-traumatic osteoarthritis (OA). This raises the possibility that orthotic control of foot motion, in an effort to attenuate this non-perpendicular motion around the axis, could prevent or minimize the resulting OA.
Several articles document the efficacy of foot orthoses for medial compartment knee pain.23 One study of patients with medial compartment knee osteoarthritis found that laterally wedged custom foot orthoses not only reduced knee pain to a greater degree than the same orthoses without the lateral wedge, but that the wedged device also reduced the peak knee adduction moment during early stance.9 Previous research has linked this pathologic adduction moment with the progression of knee osteoarthritis or the inability to fully recover from high tibial osteotomies to correct for genu varum deformities.24 Another similar study compared a laterally wedged insole with neutral insoles in patients with knee OA and found that at six months pain medication intake was significantly lower and compliance was higher in those who wore the wedged insoles.25
Overuse and ligamentous injury can be influenced by custom orthoses. A study that demonstrated this concept involved the evaluation of a group of female runners with a history of overuse running knee pain but excluded knee ligament injury.26 Custom semirigid functional foot orthoses were dispensed to the runners after impressions were taken with a neutral suspension cast. The six-week orthotic intervention produced a significant reduction in pain compared to baseline. Interestingly, the study also demonstrated that the orthoses, while reducing the pain, also increased the maximum external rotation moment at the knee and decreased maximum calcaneal eversion angle. These biomechanical effects may, in turn, reduce the peak adduction moment.9,14,23 This demonstration supports the concept that the internal rotation of the tibia, caused by subtalar and midtarsal motion, contributes to mechanically induced knee pain.
Preventive measures
Lastly, can custom orthoses control either the incidence or prevalence of ligamentous injury to the knee? Several articles27,28 demonstrated that custom devices are effective in reducing stress fractures in military recruits, and there is some evidence in the sports medicine literature this is true for ligamentous knee injuries as well.
One hundred and fifty five collegiate women’s basketball players were investigated for anterior cruciate and collateral ligament injury.22 The athletes, during a four-year period, did not use any foot orthoses during training or games. Then, for the next nine years, all team members wore foot orthoses during all basketball-related activities. The ACL was 7.14 times more likely to be injured and the collateral ligaments were 1.72 times more likely to be injured in the athletes who did not wear the orthoses. The results suggest that, by decreasing tibial internal rotation and improving timing of subtalar joint pronation, foot orthoses facilitate biomechanical alterations that lower athletes’ risk of knee ligament injury.
Orthotic goals for knee pain
Although further research may need to be more specific, existing evidence supports the use of foot orthoses not only to reduce pain in mechanically induced knee pain but also potentially to prevent knee ligament injury. There are two mechanisms that seem to be dominant in the literature. First, the rapid internal rotation of the tibia caused by early and excessive foot pronation creates a torque on the knee and positions the patella unevenly against the femur. Second, the frontal plane malalignment of the knee is exaggerated by excessive foot pronation, placing unwelcome traction on the ligaments. Foot orthoses can control and possibly reverse these scenarios by preventing unwanted foot motion or changing the frontal plane moment at the knee. 29
The goal of controlling anterior knee pain, including PFPS, can be achieved by controlling internal leg rotation using a tight-fitting, semi-rigid device that prevents calcaneal eversion and prevents midtarsal joint collapse. In my clinical experience, a semi-rigid device with a medial heel skive, flat rearfoot post and a minimal arch fill addresses these issues.
The goal of controlling medial knee pain seems to be achieved by creating a greater eversion moment at the subtalar joint axis by lateral wedging, either intrinsically or extrinsically, in an orthosis while preventing the resulting excessive midtarsal motion with a semi-rigid device. A semi-rigid device with a lateral skive, flat rearfoot post and a standard arch fill addresses these issues. (Figure 2)
The goal of preventing medial collateral ligament and ACL injuries is to limit motion in the foot. This concept has been embraced for decades in all sports through taping and strapping but logic suggests this is best accomplished with an orthotic device that controls midtarsal and subtalar motion. A more flexible device, with an arch fill, allows the device to be motion restrictive when the whole foot is on the ground but flexible at heel contact and heel lift. (Figure 3)
Regardless of the particular material used, the ability of foot orthoses to limit unwanted or compensatory motion seems to lead to reversal of symptoms and prevention of further damage. Orthotic modifications that reduce damaging moment arms and stabilize unwanted motion do produce more effective orthotic devices.
Paul R. Scherer, DPM, is the immediate past chairperson of the department of applied biomechanics at Samuel Merritt College in Oakland, CA. He is CEO of ProLab Orthotics, located in Napa, CA.
References
- Tria AJ, Palumbo RC, Alicea JA. Conservative care for patellofemoral pain. Orthop Clin North Am 1992;23(4):545-554.
- DeHaven KE, Dolan WA, Mayer PJ. Chondromalacia patellae in athletes. Clinical presentation and conservative management. Am J sports Med 1979;7(1):5-11.
- Fischer RL. Conservative treatment of patellofemoral pain. Orthop Clin North Am 1986;17(2):269-272.
- Eng JJ, Pierrynowski MR. Evaluation of soft foot orthotics in the treatment of patellofemoral pain syndrome. Phys Ther 1993;73(2):62-68.
- Nawoczenski DA, Cook TM, Saltzman CL. The effect of foot orthotics on three-dimensional kinematics of the leg and rearfoot during running. J Orthop Sports Phys Ther 1995;21(6):317-327.
- McCulloch M, Brunt D, Vander Linden D. The effect of foot orthotics and gait velocity on lower limb kinematics and temporal events of stance. J Orthop Sports Phys Ther 1993;17(1):2-10.
- Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. J Orthop Sports Phys Ther 1987;9(4):160-165.
- Mundermann A, Nigg BM, Humble RN, Stefanyshyn DJ. Foot orthotics affect lower extremity kinematics and kinetics during running. Clin Biom 2003;18(3)254-262.
- Butler RJ, Marchesi S, Royer T, Davis IS. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. J Orthop Res 2007;25(9):1121-1127.
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther 2003;33(11):639-646.
- Heiderscheit BC, Hamill J, Caldwell GE. Influence of Q-angle on lower-extremity running kinematics. J Orthop Sports Phys Ther 2000;30(5):271-278.
- D’Amico JC. The influence of foot orthoses on the quadriceps angle. J Am Podiatr Med Assoc 1986;76(6):337-340.
- Rubin R, Menz HB. Use of laterally wedged custom foot orthoses to reduce pain associated with medial knee osteoarthritis: a preliminary investigation. J Am Podiatr Med Assoc 2005;95(4):347-352.
- Collins N, Crossley K, Beller E, et al. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Br J Sports Med 2009;43(3):163-168.
- Way MC. Effects of a thermoplastic foot orthosis on patellofemoral pain in a collegiate athlete: a single-subject design. J Orthop Sports Phys Ther 1999;29(6):331-338.
- Johnston LB, Gross MT. Effects of foot orthoses on quality of life for individuals with patellofemoral pain syndrome. J Orthop Sports Phys Ther 2004;34(8):440-448.
- Pitman D, Jack D. A clinical investigation to determine the effectiveness of biomechanical foot orthoses as initial treatment for patellofemoral pain syndrome. J Prosthet Orthot. 2000;12(4);110-116.
- Saxena A, Haddad J. The effect of foot orthoses on patellofemoral pain syndrome. J Am Podiatr Med Assoc 2003;93(4):264-271.
- Beckett ME, Massie DL, Bowers KD, Stoll DA. Incidence of hyperpronation in the ACL injured knee: A clinical perspective. J Athl Train 1992;27(1):58-62.
- Woodford-Rogers B, Cyphert L, Denegar CR. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train 1994;29(4):343-346.
- Loudon JK, Jenkins WL, Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther 1996;24(2):91-97.
- Jenkins WL, Raedeke SG, Williams DS 3rd. The relationship between the use of foot orthoses and knee ligament injury in female collegiate basketball players. J Am Podiatr Med Assoc 2008;98(3):207-211.
- Brouwer RW, Jakma TS, Vehagen AP, et al. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Databse Syst Rev 2005;(1):CD004020.
- Prodromos CC, Andriacci TP, Galante JO. A relationship between gait and clinical changes following high tibial osteotomy. J Bone Joint Surg Am 1985;67(8):1188-1194.
- Maillefert JF, Hudry C, Baron G, et al. Laterally elevated wedged insoles in the treatment of medial knee osteoarthritis: a prospective randomized controlled study. Osteoarthritis Cartilage 2001;9(8):738-745.
- MacLean CL, Davis IS, Hamill J. Short and long-term influences of a custom foot orthotic intervention on lower extremity dynamics. Clin J Sport Med 2008;18(4):338-343.
- Milgrom C, Giladi M, Kashtan M, et al. A prospective study of the effect of a shock-absorbing orthotic device on the incidence of stress fractures in military recruits. Foot Ankle 1985;6(2):101-104.
- Finestone A, Giladi M, Elad H, et al. Prevention of stress fractures using custom biomechanical shoe orthoses. Clin Orthop Relat Res 1999;(360):182-190.
- Gross MT, Foxworth JL. The role of foot orthoses as an intervention for patellofemoral pain. J Orthop Sports Phys Ther 2003;33(11):661-670.
Table 1. Orthotic Recommendations for PFPS
- Neutral suspension cast
- Semi-rigid polypropylene device
- Balanced positive to perpendicular
- Minimum cast fill to control forefoot to rearfoot motion
- Rearfoot posting
- 2mm medial skive, especially with an everted calcaneus
- A topcover that adjusts to the patient’s shoe gear or athletic footwear
Table 2. Orthotic Recommendations for Medial Compartment Knee Pain
- Neutral suspension cast
- Semi-rigid polypropylene
- Balance positive to perpendicular
- Standard cast fill
- Rearfoot post
- 12mm heel cup
- 4 mm lateral skive
- Topcover consistent with patient’s shoes and activity
Table 3. Orthotic Recommendations for Knee Ligament Prophylaxis
- Neutral suspension cast
- Semi-rigid polypropylene
- Positive cast correction balanced to perpendicular
- Minimum cast fill
- EVA orthotic arch fill
- 12mm heel cup
- Flat rearfoot post
- No bevel rearfoot post
- Topcover consistent with patient’s shoes and activity











Trackbacks/Pingbacks