There is a notable risk of prolonged opioid use in older patient populations following musculoskeletal injury according to a new study presented at the 2021 Annual Meeting of the American Academy of Orthopaedic Surgeons. While numerous studies have analyzed opioid dependence in younger patient cohorts, relatively few studies have examined the risk factors and prevalence associated with long-term opioid usage in patients age 60 and older, who, despite their age, remain at risk for opioid dependence.
There is a notable risk of prolonged opioid use in older patient populations following musculoskeletal injury according to a new study presented at the 2021 Annual Meeting of the American Academy of Orthopaedic Surgeons. While numerous studies have analyzed opioid dependence in younger patient cohorts, relatively few studies have examined the risk factors and prevalence associated with long-term opioid usage in patients age 60 and older, who, despite their age, remain at risk for opioid dependence.
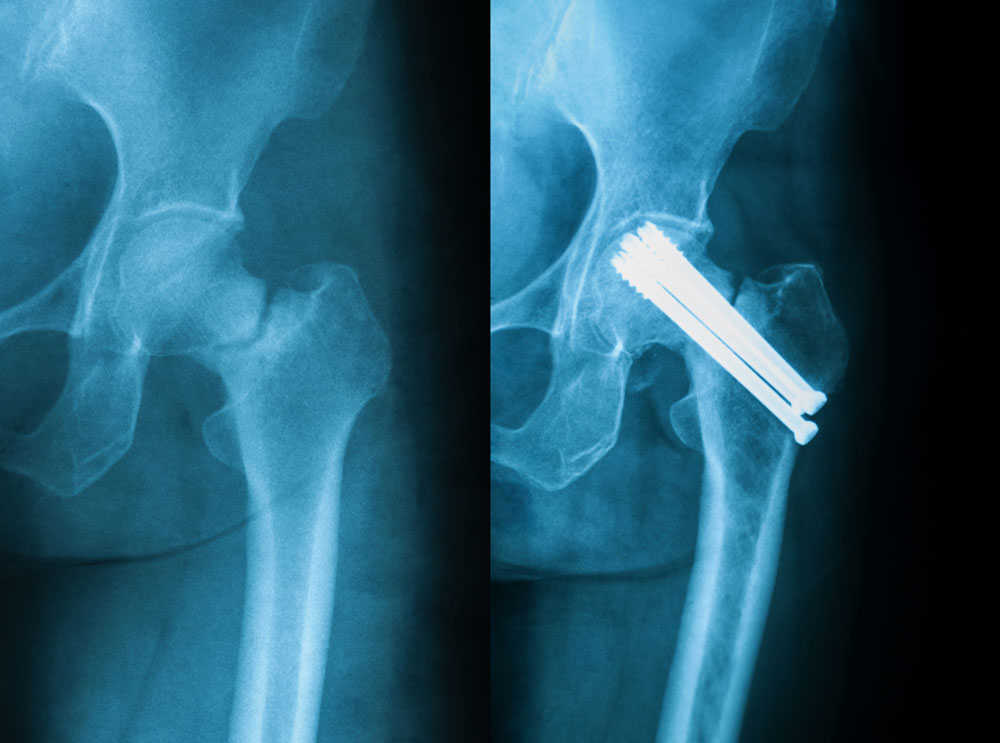
The retrospective cohort study, “Prolonged Opioid Usage Following Hip Fracture Surgery in Opioid-Naïve Older Patients,” followed 29,618 opioid-naïve patients (not filling an opioid prescription 3 months prior to the hip fracture), age 60 and older, who underwent surgical treatment of a hip fracture between 2009 and 2018. The research team, led by Kanu Okike, MD, MPH, FAAOS, used Kaiser Permanente’s Hip Fracture Registry for the study. Because the registry uses a patient’s electronic medical records, the research team was also able to capture relevant factors such as demographics, preexisting comorbidities, and opioid use before, during, and after surgery.
With these data, the study looked at outpatient opioid use during 3 time periods — 0 to 30 days post-surgery (P1), 31 to 90 days post-surgery (P2), and 91 to 180 days post-surgery (P3) — to analyze prolonged outpatient opioid use, defined as filling one or more opioid prescriptions in all 3 time periods.
“Hip fractures stand alone not only in their frequency among older adults, but because they increase the risk of morbidity and mortality,” said Okike, lead researcher and orthopaedic trauma surgeon at Hawaii Permanente Medical Group in Honolulu. “Given that hip fractures are a severe injury in an already frail patient population, it would be problematic if some patients were also developing opioid dependence following their injury.”
Of patients who remained alive for the entire study, the proportion of outpatient opioid usage was 83.7% (24,776/29,618) in P1, 69% (19,380/28,068) in P2, and 16.7% (4,435/26,481) in P3. Of note, the team found that that 1 in 6 elderly hip fracture patients were still taking opioid pain medications at 3 to 6 months following hip fracture surgery.
Additional findings include:
- Prolonged opioid usage was less commonly observed among patients who were either Asian, had an annual income of $150,000 or greater, or had undergone regional anesthesia.
- The most common types of opioid prescriptions filled in the 6 months following hip fracture surgery were hydrocodone (53.9%), oxycodone (22.4%), and morphine (6.8%).
- Prolonged opioid usage was more common following fracture fixation and less common following total hip arthroplasty (both in comparison to hemiarthroplasty).
“While most of the concerns and opioid usage research in elderly individuals have centered on short term risks, such as oversedation and delirium, our findings suggest that prolonged opioid usage is an important concern in this older population, just as in the younger trauma populations,” said Okike. “Our hope is that by uncovering more data and continuing to educate patients of all ages, the orthopaedic community will be able to better aid efforts to decrease long-term opioid dependence in their patients.”