 Full-length carbon graphite orthoses may improve outcomes in patients who have tried three-quarter length orthoses without symptomatic relief. Research suggests the key factors are load redistribution and forefoot motion control.
Full-length carbon graphite orthoses may improve outcomes in patients who have tried three-quarter length orthoses without symptomatic relief. Research suggests the key factors are load redistribution and forefoot motion control.
by Smita Rao, PT, PhD
Arthritis of the tarsometatarsal joints (midfoot) has emerged as a significant clinical challenge due to its increasing incidence compounded by high potential for chronic secondary disability. The etiology of midfoot arthritis includes primary, inflammatory and post-traumatic causes.1,2 Midfoot injuries have been estimated to affect approximately 55,000 people per year in the United States.2 However, as many as 20% of tarso-metatarsal joint injuries are missed during initial examination.3-5 Due to the multiple complex articulations that comprise the midfoot, even minimal disruption is indicative of significant injury.
While midfoot injuries are frequently reported in the athletic population, the occurrence of these injuries secondary to motor vehicle trauma has increased in frequency as well as severity.6-9 Since the advent of automobile airbags, the increased incidence of midfoot injuries following vehicular trauma has been attributed to high impact forces sustained with the foot against the floorboard.3,10 In addition, as our population ages, the long-term effects of chronic increased joint loads sustained with high heeled footwear may also contribute to the development and progression of degenerative midfoot arthritis.11 Irrespective of the mechanism of trauma, midfoot arthritis has been reported to be the inevitable sequelae of tarsometatarsal disease.
Non-operative management
Patients with midfoot arthritis experience moderate to severe foot pain, which may limit their participation in walking and recreational physical activity. Operative intervention in the form of arthrodesis is challenging due to the complex anatomy of the midfoot region. While surgical intervention has been associated with decreased pain, there have been surprisingly modest improvements in function.3,10,12-15 For these reasons, non-invasive conservative management in the form of foot orthoses serves as a particularly valuable first line of treatment in this population.
Patients with midfoot arthritis present with foot pain that is localized to the medial tarsometatarsal joints and aggravated by weight-bearing. Concomitant radiographic changes include degenerative changes at the tarsometatarsal joints reflected in joint space narrowing, dorsal bossing and osteophyte formation.16,17 Previous reports have also found radiographic evidence of pes planovalgus foot alignment in patients with midfoot arthritis.18 Consistent with these findings, the goal of orthotic intervention is to achieve pain relief by limiting motion at the painful tarsometatarsal joints and restoring optimal arch alignment. To this end, arch-restoring devices such as the custom-molded three-quarter length orthoses (3Q) are frequently prescribed in this population. The rationale guiding 3Q prescription is that the design features of the 3Q, such as its arch build up and contoured heel, will favorably influence foot kinematics and thus afford pain relief.19-21
Evaluating the effect of orthoses
Evidence in support of using 3Q orthoses in patients with low arch alignment comes from studies documenting improved control of calcaneal motion 22-25 and arch alignment26 accompanying 3Q use during walking. In a prospective randomized clinical trial of orthoses in patients with rheumatoid arthritis and painful correctable rearfoot valgus deformity, Woodburn et al demonstrated significant reduction in foot pain and decreased calcaneal eversion with use of 3Q orthoses.27,28
In contrast to the favorable outcomes that have been reported, our clinical experience suggests that patients with midfoot arthritis continue to report pain despite 3Q use. As an alternative, the full length (FL) carbon graphite orthosis, an over-the-counter device, has been proposed. The recommendation is based on reports from patients with arthritis of the 1st metatarsophalangeal joint (hallux rigidus),29,30 where the FL orthosis has been postulated to control 1st metatarsophalangeal joint (MTP1) motion and consequent 1st metatarsal (MT1) motion during walking, and prevent mechanical impingement on the dorsal aspect of the MTP1 joint. Since MT1 forms the distal articular surface of the tarsometatarsal complex, use of the FL orthosis may limit MT1 motion during walking and potentially prevent dorsal impingement at the tarsometatarsal complex.
In addition to altering foot alignment, 3Q inserts also alter regional plantar loading.31-33 Custom molded inserts decrease plantar loading at the forefoot and heel and increase plantar loading at the midfoot.31-33 Load transfer mechanisms have been associated with favorable functional outcomes in patients with forefoot pathology such as rheumatoid arthritis, diabetes, and painful pes cavus.31,34 However, in our experience, functional outcomes following the use of 3Q inserts in patients with midfoot arthritis have not been as positive. In our study of 30 patients with midfoot arthritis, 21 were previous users of the 3Q inserts but continued to experience pain.35
While the design features of the 3Q insert facilitate pain relief in patients with forefoot pathology, the load transfer accompanying their use may be detrimental to patients with midfoot pathology. Previous studies have reported modest relationships between pain and plantar loading,36,37 and Burns et al31 reported a significant positive relationship between total foot pressure time integral and foot pain in patients with rigid high arches secondary to pes cavus foot deformity.31 Similarly, unpublished data from our laboratory (currently in review) indicate a modest positive relationship between medial midfoot loading sustained during barefoot walking and self-reported pain in patients with midfoot arthritis. Ours is the first study to report a relationship between regional plantar loading and self-reported pain in patients with midfoot arthritis.
To address gaps in current knowledge, we undertook two studies. The purpose of the first study was to identify kinematic impairments in patients with midfoot arthritis, compared to age- gender- and BMI-matched control subjects. The purpose of the second study was to assess the effect of a four-week intervention with FL orthoses on self-reported functional outcomes, plantar loading and in vivo foot kinematics in patients with midfoot arthritis.
Research findings
All procedures were approved by the review boards of the University of Rochester and Ithaca College; informed consent was sought prior to initiating study procedures. All data were collected at the Movement Analysis Lab at the Department of Physical Therapy, Ithaca College – Rochester Center, Rochester, NY.
We recruited 30 patients with midfoot arthritis and 20 control subjects, matched in age, gender and BMI. All patients sought care at the the University of Rochester Medical Center. All patients presented with unilateral symptoms, comprising pain on the dorsum of the foot, localized to the tarsometatarsal region and aggravated by weight-bearing. The diagnosis of isolated midfoot arthritis was confirmed by radiographic evidence of degenerative changes at one or more tarsometatarsal joints on antero-posterior and lateral weight-bearing x-rays. A single fellowship-trained foot and ankle orthopedic surgeon screened all subjects. None of the patients recollected a traumatic event preceding their symptoms. Control subjects were recruited from the community using fliers, screened by a single trained physical therapist (SR) for lower extremity pain and/or dysfunction and matched for age, gender and BMI to patients with midfoot arthritis. In vivo segmental foot motion was assessed using a previously developed foot model.38,39
All patients were given one pair of FL orthoses at initial evaluation. These were over-the-counter inserts, made of carbon graphite. The orthoses were full length, extending from the heel to the tip of the toe; semi-rigid (according to manufacturer’s specifications), with an average thickness of 1.59 mm; and featured no arch buildup or contoured heel. Patients were encouraged to wear the FL during all weight bearing activities.
Following a four-week intervention with the FL, patients with midfoot arthritis demonstrated statistically significant and clinically relevant change, as discerned using a region-specific outcomes instrument, the Foot Function Index – Revised.35 This measurement tool assesses self-reported foot function in the following dimensions: pain, stiffness, activity limitation, psychosocial issues.
Impairments in segmental foot motion
A comparison of segmental foot motion during barefoot walking and step descent confirmed that step descent required greater MTP1dorsiflexion, MT1 plantar flexion, ankle dorsiflexion, calcaneus eversion and forefoot abduction than walking, in both study and control groups. In addition, step descent also necessitated greater range of motion for MTP1 dorsiflexion, ankle dorsiflexion and forefoot abduction in both groups.
A key finding of this study, with potential clinical ramifications, is that patients with midfoot arthritis responded differently to the step task compared to control subjects in terms of MT1 and calcaneus eversion ROM. Increased MT1 plantar flexion and calcaneal eversion ROM in the step activity was noted in patients with midfoot arthritis.38 As expected, peak motion during the step task was greater than during walking, in both groups [ two way interaction not statistically significant]. However total peak to peak motion (excursion) was different in the two groups, and during the two tasks [two way interaction statistically significant]. Patients with midfoot arthritis demonstrated significantly less MT1 motion during walking compared to the control subjects, which may represent a “stiffening strategy” to limit articular stress at the tarsometatarsal joints, because the MT1 forms the distal part of the tarsometatarsal articulation. In the step task, however, both groups showed similar MT1 plantar flexion range of motion.38 The inability to modulate MT1 plantar flexion ROM during the step task may contribute to pain elicited during the task. The increased range of MT1 motion in step descent compared to walking in patients with midfoot arthritis may be indicative of loss of midfoot stability, evident only in more challenging non-gait activities.
Calcaneal eversion was significantly greater in midfoot arthritis patients than in controls during step descent but not during walking. This finding contrasts with Woodburn’s finding that decreased calcaneal eversion was associated with less pain in rheumatoid arthritis patients,27,28 underscoring the differences between the two patient populations.
Effect of orthoses on foot motion
Use of the FL orthoses resulted in decreased MTP1 and MT1 range of motion during walking, compared to the shoe-only condition. Improved control of MT1 and MTP1 motion may be a key factor mediating pain relief in patients with midfoot arthritis. Our findings suggest that the FL orthoses may mimic a “stiffening strategy” by restricting MTP1 joint dorsiflexion range of motion and MT1 plantar flexion range of motion during walking compared to the shoe-only condition. The stiffening strategy, reflected in reduced MT1 motion, may be particularly valuable in patients with early degenerative changes, who may subject their feet to more physical activity and consequent joint stress, due to their higher level of physical functioning.
Effect of orthoses on plantar loading
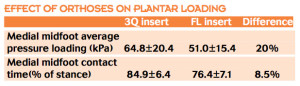 In terms of plantar loading, use of the FL insert was accompanied by 20% decrease in magnitude and 8.5% decrease in duration of medial midfoot loading compared to the 3Q insert, based on the aforementioned fact that 70% of patients were previous users of 3Q inserts. Degenerative disorders of the foot, such as arthritis, may render the foot more susceptible to pain either through mechanical over-loading of plantar regions that are not usually loaded, or because the foot has a lower tolerance to normal plantar loading. Regional plantar loading may contribute to the development of symptoms by directly stimulating mechanoceptors and nociceptors in the plantar aspect of the foot. Additionally, they may also have indirect consequences on the reaction forces and moments, reflective of articular loading sustained at the tarsometatarsal joints.
In terms of plantar loading, use of the FL insert was accompanied by 20% decrease in magnitude and 8.5% decrease in duration of medial midfoot loading compared to the 3Q insert, based on the aforementioned fact that 70% of patients were previous users of 3Q inserts. Degenerative disorders of the foot, such as arthritis, may render the foot more susceptible to pain either through mechanical over-loading of plantar regions that are not usually loaded, or because the foot has a lower tolerance to normal plantar loading. Regional plantar loading may contribute to the development of symptoms by directly stimulating mechanoceptors and nociceptors in the plantar aspect of the foot. Additionally, they may also have indirect consequences on the reaction forces and moments, reflective of articular loading sustained at the tarsometatarsal joints.
Summary and conclusions
Taken together, the recent reports provide quantitative data delineating impairments in segmental foot motion in patients in midfoot arthritis. FL orthoses may redistribute loads at the plantar surface of the foot and offer increased control of MTP1 motion in patients with midfoot arthritis. Orthotic management seems to work well, even for patients with early stages of arthritis. Although none of the midfoot arthritis patients we studied reported a precipitating traumatic event, it is possible that in patients with acute midfoot injuries, orthotic management can delay progression of symptoms and also alleviate symptoms.
The effect of foot orthoses in patients with midfoot arthritis may also depend on foot structure. Davitt et al proposed that the length of the second metatarsal relative to the first metatarsal is significantly longer in patients with midfoot arthrosis than in control subjects;40 this “Morton’s Foot” structure has been linked to other types of foot pathology as well, suggesting that it may be a sensitive but non-specific indication of abnormal mechanics. We are currently analyzing our data to look for mechanisms by which a functionally longer second metatarsal may influence foot function.
Smita Rao, PT, PhD, is an assistant professor in the department of physical therapy at New York University, New York, NY. This work was performed as part of her post-doctoral fellowship when she was a scholar-in-residence at the Center for Foot and Ankle Research in the department of physical therapy at Ithaca College-Rochester Center, Rochester, NY.
Acknowledgements:
We would like to acknowledge funding support from the Arthritis Foundation and the American Orthopaedic Foot and Ankle Society. 15 full length carbon graphite shoe inserts were donated by Wrymark, Inc.
Statement of financial disclosure and conflict of interest statement:
The author of this manuscript affirms that she has no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript except as cited in the manuscript.
References:
1. Myerson MS, Cerrato RA. Current management of tarsometatarsal injuries in the athlete. J Bone Joint Surg Am 2008;90(11):2522-2533.
2. Hardcastle PH, Reschauer R, Kutscha-Lissberg E, Schoffmann W. Injuries to the tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg Br 1982;64(3):349-356.
3. Arntz CT, Hansen ST, Jr. Dislocations and fracture dislocations of the tarsometatarsal joints. Orthop Clin North Am 1987;18(1):105-114.
4. Goossens M, De Stoop N. Lisfranc’s fracture-dislocations: etiology, radiology, and results of treatment. A review of 20 cases. Clin Orthop Relat Res 1983;(176):154-162.
5. Englanoff G, Anglin D, Hutson HR. Lisfranc fracture-dislocation: a frequently missed diagnosis in the emergency department. Ann Emerg Med 1995;26(2):229-233.
6. Manoli A 2nd, Prasad P, Levine RS. Foot and ankle severity scale (FASS). Foot Ankle Int 1997;18(9):598-602.
7. Richter M, Thermann H, Wippermann B, et al. Foot fractures in restrained front seat car occupants: a long-term study over twenty-three years. J Orthop Trauma 2001;15(4):287-293.
8. Parenteau CS, Viano DC, Lovsund P, Tingvall C. Foot-ankle injuries: influence of crash location, seating position and age. Accid Anal Prev 1996;28(5):607-617.
9. Wilson LS Jr., Mizel MS, Michelson JD. Foot and ankle injuries in motor vehicle accidents. Foot Ankle Int 2001;22(8):649-652.
10. Richter M, Wippermann B, Krettek C, et al. Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot Ankle Int 2001;22(5):392-398.
11. Yu J, Cheung JT, Fan Y, et al. Development of a finite element model of female foot for high-heeled shoe design. Clin Biomech 2008;23 Suppl 1:S31-S38.
12. Teng AL, Pinzur MS, Lomasney L, et al. Functional outcome following anatomic restoration of tarsal-metatarsal fracture dislocation. Foot Ankle Int 2002;23(10):922-926.
13. Kuo RS, Tejwani NC, Digiovanni CW, et al. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am 2000;82(11):1609-1618.
14. Ly TV, Coetzee JC. Treatment of primarily ligamentous Lisfranc joint injuries: primary arthrodesis compared with open reduction and internal fixation. A prospective, randomized study. J Bone Joint Surg Am 2006;88(3):514-520.
15. Arntz CT, Veith RG, Hansen ST Jr. Fractures and fracture-dislocations of the tarsometatarsal joint. J Bone Joint Surg Am 1988;70(2):173-181.
16. Myerson MS, Fisher RT, Burgess AR, Kenzora JE. Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot Ankle 1986;6(5):225-242.
17. Rao S, Nawoczenski DA, Baumhauer JF. Midfoot arthritis: nonoperative options and decision making for fusions. Techniques in Foot & Ankle Surgery 2008;7(3):188-195.
18. Jung HG, Myerson MS, Schon LC. Spectrum of operative treatments and clinical outcomes for atraumatic osteoarthritis of the tarsometatarsal joints. Foot Ankle Int 2007;28(4):482-489.
19. Clark H, Rome K, Plant M, et al. A critical review of foot orthoses in the rheumatoid arthritic foot. Rheumatology 2006;45(2):139-145.
20. Shrader JA. Nonsurgical management of the foot and ankle affected by rheumatoid arthritis. J Orthop Sports Phys Ther 1999;29(12):703-717.
21. Janisse DJ, Janisse E. Shoe modification and the use of orthoses in the treatment of foot and ankle pathology. J Am Acad Orthop Surg 2008;16(3):152-158.
22. Zifchock RA, Davis I. A comparison of semi-custom and custom foot orthotic devices in high- and low-arched individuals during walking. Clin Biomech 2008;23(10):1287-1293.
23. Novick A, Kelley DL. Position and movement changes of the foot with orthotic intervention during the loading response of gait. J Orthop Sports Phys Ther 1990;11(7):301-312.
24. Branthwaite HR, Payton CJ, Chockalingam N. The effect of simple insoles on three-dimensional foot motion during normal walking. Clin Biomech 2004;19(9):972-977.
25. Nester CJ, van der Linden ML, Bowker P. Effect of foot orthoses on the kinematics and kinetics of normal walking gait. Gait Posture 2003;17(2):180-187.
26. Nawoczenski DA, Ludewig PM. The effect of forefoot and arch posting orthotic designs on first metatarsophalangeal joint kinematics during gait. J Orthop Sports Phys Ther 2004;34(6):317-327.
27. Woodburn J, Barker S, Helliwell PS. A randomized controlled trial of foot orthoses in rheumatoid arthritis. J Rheumatol 2002;29(7):1377-1383.
28. Woodburn J, Helliwell PS, Barker S. Changes in 3D joint kinematics support the continuous use of orthoses in the management of painful rearfoot deformity in rheumatoid arthritis. J Rheumatol 2003;30(11):2356-2364.
29. Nawoczenski DA, Ketz J, Baumhauer JF. Roger Mann Award: Dynamic kinematic and plantar pressure changes forllowing cheilectomy for hallux rigiidus – a long-term follow-up. Foot and Ankle International. Accepted.
30. Sammarco VJ, Nichols R. Orthotic management for disorders of the hallux. Foot Ankle Clin 2005;10(1):191-209.
31. Burns J, Crosbie J, Hunt A, Ouvrier R. The effect of pes cavus on foot pain and plantar pressure. Clin Biomech 2005;20(9):877-882.
32. Bus SA, Ulbrecht JS, Cavanagh PR. Pressure relief and load redistribution by custom-made insoles in diabetic patients with neuropathy and foot deformity. Clin Biomech 2004;19(6):629-638.
33. Lott DJ, Hastings MK, Commean PK, et al. Effect of footwear and orthotic devices on stress reduction and soft tissue strain of the neuropathic foot. Clin Biomech 2007;22(3):352-359.
34. van der Leeden M, Steultjens M, Dekker JH, et al. Forefoot joint damage, pain and disability in rheumatoid arthritis patients with foot complaints: the role of plantar pressure and gait characteristics. Rheumatology 2006;45(4):465-469.
35. Rao S, Baumhauer JF, Becica L, Nawoczenski DA. Shoe inserts alter plantar loading and function in patients with midfoot arthritis. J Orthop Sports Phys Ther 2009;39(7):522-531.
36. Hodge MC, Bach TM, Carter GM. novel Award First Prize Paper. Orthotic management of plantar pressure and pain in rheumatoid arthritis. Clin Biomech 1999;14(8):567-575.
37. Jannink M, van Dijk H, Ijzerman M, et al. Effectiveness of custom-made orthopaedic shoes in the reduction of foot pain and pressure in patients with degenerative disorders of the foot. Foot Ankle Int 2006;27(11):974-979.
38. Rao S, Baumhauer JF, Tome J, Nawoczenski DA. Comparison of in vivo segmental foot motion during walking and step descent in patients with midfoot arthritis and matched asymptomatic control subjects. J Biomech 2009;42(8):1054-1060.
39. Rao S, Saltzman C, Yack HJ. Segmental foot mobility in individuals with and without diabetes and neuropathy. Clin Biomech 2007;22(4):464-471.
40. Davitt JS, Kadel N, Sangeorzan BJ, et al. An association between functional second metatarsal length and midfoot arthrosis. J Bone Joint Surg Am 2005;87(4):795-800.










good information for me. At 77 it’s really no fun. Always been physcially active a d now don’t do too much. every other month I serve at church as a Comforter for Homegoings.(funerals}. Those days which are at least 3 per wk We stand and assist family members. It is getting very difficult to stand without hold up my left foot. Dr. put me ina boot , it was too heavy made my hip hurt. Now I have one that fits in shoe and straps around ankle. Can not take this too long. I am going to order the ortha;heel shoes and the support for inside shoes on my own. I really don’t like the pain and I’m alerjic to even asprin so I don’t want any medication. Thanks for this info.