 By CPT Jamie B. Morris, DPT, OCS, CSCS, and LTC Donald L. Goss, PT, PhD, OCS, ATC
By CPT Jamie B. Morris, DPT, OCS, CSCS, and LTC Donald L. Goss, PT, PhD, OCS, ATC
Study findings suggest that increased loading rates and tibial acceleration are associated with an increased risk of sustaining a tibial stress fracture. Interventions directed at reducing these impact variables may decrease the incidence and recurrence of this serious injury.
Stress fractures are a common overuse injury of the bone attributed to the repetitive strain associated with impact activities such as running and marching.1 Stress fractures are among the most common injuries sustained by runners and military populations. They are among the top 10 overuse injuries and account for up to 50% of all injuries in runners and military recruits, with an annual incidence of up to 31%.2,3
The tibia is the most commonly injured bone and accounts for 33% to 55% of stress fractures.2 Tibial stress fractures (TSF) have one of the highest recurrence rates, ranging from 10.6% to 36% in military recruits.2 TSF are also associated with a long recovery period, often requiring up to 12 weeks of activity modification.4 This can lead to diminished cardiovascular fitness in soldiers and athletes due to reduced training.5 TSF not only result in a loss of physical fitness, but also result in considerable financial loss, including an estimated $6.2 million annually related to US Army recruits discharged from basic training due to this injury.6
It is important to understand the etiology of the injury and appropriate management and preventive methods to reduce the incidence of TSF and its rate of recurrence. Stress fractures often develop because of multiple influences, such as biomechanical, hormonal, nutritional, and genetic factors.1 An understanding of the pathophysiology, epidemiology, biomechanics, and diagnosis, as well as modifiable risk factors, can help practitioners take steps to reduce the incidence and recurrence of this costly injury.
Pathophysiology
During weight-bearing and impact activities such as running and marching, the skeleton is exposed to mechanical loading, which causes bone to deform. The amount of deformation depends on the magnitude of the load and the ability of the bone to resist deformation, or strain. The amount of strain caused by running and marching is much smaller than the degree required to fracture cortical bone, but is still capable of causing microdamage over time.7
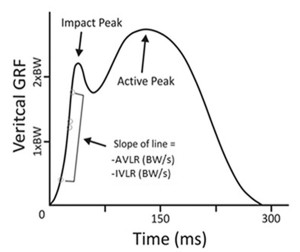
Figure 1. Vertical ground reaction force (GRF) curve with the variables of interest, average vertical loading rate (AVLR) and instantaneous vertical loading rate (IVLR). Note that both vertical loading rates (AVLR and IVLR) were calculated in the region between 20% and 80% of the impact peak. (Adapted from http://runblogger.com/ 2011/02/vertical-impact-loading-rate-in-running.html.)
Wolff’s law states that bone remodeling is a response to applied mechanical stress. It is a function of the number of loading cycles, cycle frequency, and the amount of strain.1 Bone remodels though continuous osteoclastic and osteoblastic activity that occurs throughout life. Remodeling normally repairs microdamage as it occurs, and osteoblasts deposit new bone to create a new structural unit that can withstand greater loads. This adaptation decreases the degree of bone strain associated with a given load, so greater loads are tolerated without microdamage formation.7 However, if excessive loads or cycles continue at a faster rate than skeletal repair can be maintained, a stress injury will occur because of excessive bone strain and the accumulation of microdamage.1
Epidemiology
TSF occur most frequently in association with high-impact activities due to the repetitive mechanical loading of the bone. The greatest incidence of tibial stress injuries has been reported in long distance runners and military populations.8 One third of cross-country runners report a history of stress fracture, and the sport’s annual incidence can be as high as 21%. Of those reported, half occur in the tibia. Meanwhile, 10% to 12% of those athletes will sustain another stress injury within two years.9,10 The literature is mixed on the difference in incidence rates between male and female athletes. Bennell et al demonstrated no difference in incidence between male and female track and field athletes in a one-year prospective study.9 Arendt el al, however, found the incidence of stress fractures in female collegiate athletes was double that of their male peers.11
The reported incidence of stress fractures among US military trainees is 4.8%12 to 19%,13 and as high as 31% in Israeli trainees.14 It is more common in military populations for women to sustain a stress injury; a female recruit is 3.5 times more likely to develop a stress injury than a male recruit.15 Lastly, older military recruits are more likely to sustain a stress injury than their younger counterparts. The risk of injury increases to 5% for Army recruits older than 29 years,15 and Marine recruits older than 21 years are twice as likely as younger recruits to develop a stress fracture.16 The recurrence rate for stress fractures in a military training population is also considerable, ranging from 10.6% to 36%.2,3
Risk factors
 With such a high incidence and rate of recurrence, it is important to understand the risk factors for stress fractures to prevent and manage these injuries. The cause of stress fractures is multifactorial, but ultimately depends on the bone’s ability to resist deformation. Therefore, risk factors can be divided into extrinsic factors, which refer to the loads that cause deformation when applied to the bone, and intrinsic factors, which refer to the ability of the bone to resist a load.1,7 Extrinsic factors include training regimen, footwear, training surface, and biomechanical factors.1 Intrinsic factors include gender, age, race, diet, and endocrine status. This review focuses on the biomechanical extrinsic risk factors that are associated with TSF.
With such a high incidence and rate of recurrence, it is important to understand the risk factors for stress fractures to prevent and manage these injuries. The cause of stress fractures is multifactorial, but ultimately depends on the bone’s ability to resist deformation. Therefore, risk factors can be divided into extrinsic factors, which refer to the loads that cause deformation when applied to the bone, and intrinsic factors, which refer to the ability of the bone to resist a load.1,7 Extrinsic factors include training regimen, footwear, training surface, and biomechanical factors.1 Intrinsic factors include gender, age, race, diet, and endocrine status. This review focuses on the biomechanical extrinsic risk factors that are associated with TSF.
Biomechanical factors can be subdivided into those related to abnormal loads applied to a normally aligned bone and those related to abnormal motion from normal forces applied to an abnormally aligned bone.7 Multiple studies provide evidence that abnormal loading is associated with an elevated risk of TSF. Abnormal loading may be attributed to increased ground reaction forces (GRF), loading rates, tibial acceleration, and free moments.
GRF is the force exerted on a body by the ground it is in contact with (Figure 1). Typical peak vertical GRF with running is between 1.5 and 3.5 times body weight (BW).17 There is minimal evidence that GRF magnitude is associated with the risk of TSF.18–20 However, there is both retrospective and prospective evidence that GRF loading rates are associated with TSF.
Average vertical loading rate (AVLR) and instantaneous vertical loading rate (IVLR) refer to the amount of time it takes from initial contact to the first impact peak on a GRF curve (Figure 1)—in other words, how quickly the impact force is applied to the body. In two retrospective studies,20,21 individuals with a history of TSF were matched for age and running mileage to individuals without a history of stress fracture. Those with a history of stress fracture had significantly greater AVLR and IVLR than those without. Prospectively, Davis et al22 also identified a greater AVLR and IVRL in female runners who went on to develop a TSF.
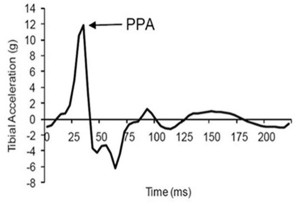
Figure 2. Peak positive acceleration (PPA), the highest acceleration measurement on a tibial acceleration curve during stance phase of running. (Reprinted with permission from reference 6.)
Another abnormal loading variable attributed to TSF is tibial acceleration. An accelerometer strapped to the tibia can measure the physical acceleration of the tibia during stance phase of running (Figure 2). The variable of interest is the peak positive acceleration (PPA), or the highest acceleration measurement during stance phase on a tibial acceleration curve.20 Retrospectively, Milner et al20 and Pohl et al21 determined that female runners with a history of TSF had greater PPA (by almost 2 g) than matched controls. They accurately predicted group membership 70% of the time based on the magnitude of PPA.20 Prospectively, Davis et al22 detected a PPA almost two times greater in female runners who later developed a TSF compared with matched controls.
Free moment has also been associated with tibial stress fractures. This is the torque about a vertical axis due to the friction between the foot and the ground during stance phase of running. Free moment acts to resist foot abduction (toeing out) during the first 70% of the support phase of stance and resists foot adduction (toeing in) during the late support phase of stance (Figure 3).18,19 This results in a torsional load applied to the tibia. Milner et al19 and Pohl et al21 reported significantly greater free moment in runners with a history of TSF compared with matched controls. They were able to accurately predict group membership 66% of the time based on the magnitude of free moment.19
Running requires greater range of motion than walking to ease large ground reaction forces, so joint kinematics have been studied to identify risk factors associated with TSF. Pohl et al21 reported greater peak hip adduction, peak knee internal rotation, and peak rearfoot eversion in runners with a history of TSF. The joint kinematic variables combined with free moment had a significant predictive relationship for stress fracture. The combination of hip adduction, knee internal rotation, rearfoot eversion, and free moment correctly classified 83% of runners into the appropriate group. Lastly, Cameron et al23 demonstrated prospectively that knee valgus and internal rotation during a jump-landing task are associated with a two- to four-times greater incidence of lower extremity stress fractures.
Diagnosis
Individuals with a TSF often have a predictable history that includes the gradual onset of pain, typically described as a diffuse ache that worsens with continued impact activity. Often, the patient has recently increased their training intensity or frequency. A physical exam reveals localized tenderness to palpation of the tibia with well-defined anatomical borders. Symptoms may also be elicited with provocative testing, such as a single-leg hop.7,24 Lastly, imaging may be used for definitive diagnosis. Plain radiographs should be used first because they are inexpensive and readily available. It is important to note that, in the first week of symptoms, the sensitivity of radiographs for TSF is only 10%; this increases to 56% after five weeks.25 A bone scan may be used for its high sensitivity (74%-100%), but it has a low specificity that may result in a false positive result.25 Magnetic resonance imaging is the gold standard for stress fracture imaging, as it has a sensitivity of 88% to 100% and a specificity of 86% to 100%.25,26
Management
Once a stress fracture is identified, it is important to remove the patient immediately from impact activity. If necessary, weight bearing may be reduced with crutches for pain control. After four to 12 weeks of activity modification, when patients can walk without pain for three to five days, they may gradually return to impact activities.7,11,24 Due to the recurrent nature of stress fractures, this is the ideal time to identify and address biomechanical risk factors, such as loading rates and tibial acceleration. Recent evidence supports gait retraining to alter these risk factors by modifying step length, step frequency, and tibial shock.
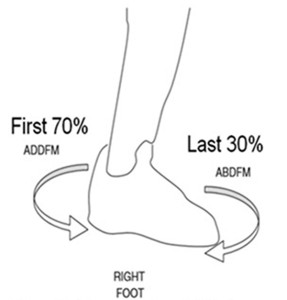
Figure 3. Representation of adduction free moment (ADDFM) resisting toe out and abduction free moment (ABDFM) resisting toe in of the foot during stance phase of running. (Adapted from reference 20.)
Crowell et al6 demonstrated that runners at risk for TSF are able to decrease loading variables with the use of real-time visual feedback. They identified 10 runners with elevated PPA (greater than 8 g), and trained them in eight sessions over two weeks. The runners were provided with real-time visual feedback of their tibial shock and were instructed to “run softer” to decrease their PPA by at least 50%. A faded feedback approach was used in which the amount of feedback provided was gradually decreased in the last four training sessions. After two weeks, there was a significant reduction in AVLR, IVLR, and PPA compared with baseline levels. These changes were also maintained at one month.
Clansey et al27 also demonstrated that real-time feedback aimed at reducing tibial shock results in decreased loading variables. He recruited 22 male runners with elevated PPA (greater than 9 g), and randomized them into a real-time feedback training (RTF) group or a control group. Both groups performed six 20-minute treadmill runs over three weeks. The RTF group received both visual and audio feedback on their tibial shock, and runners in this group were instructed to “find a strategy” to decrease their PPA by 50%. After three weeks, AVLR, IVLR, and PPA in the RTF group were significantly lower than baseline and also lower than in the control group. However, only PPA remained significantly reduced at the one-month follow-up. The authors suggested this might be due to the lack of faded feedback, as the participants received constant feedback in each session.
Willy et al28 demonstrated that altering step frequency resulted in decreased loading variables. They recruited 30 runners with increased IVLR (greater than 85 BWs), and randomized them into a retraining group or a control group. Runners in each group were issued a GPS watch and instructed to continue to run their normal mileage. Runners in the retraining group also received an accelerometer that transmitted the runner’s step rate to the watch. Runners were instructed to maintain a step rate 7.5% above their preferred baseline step rate. A faded feedback approach was used in which the runners in the retraining group only used the watch for runs one through three and runs five and seven. After eight training runs, step rate, AVLR, IVLR, peak hip adduction, and eccentric knee work in the retraining group were significantly lower than baseline levels and also lower when compared with the control group. These changes were maintained at a one-month follow-up.
Conclusion
Tibial stress fractures are one of the most common overuse injuries in athletes and military populations due to impact activity such as running and marching. They occur due to the accumulation of microdamage from repetitive loading of the bone. Due to the recurrent nature of stress fractures, it is important to understand the potential biomechanical contributors to this injury. There is evidence that increased loading rates and tibial acceleration place an individual at increased risk of sustaining a TSF. Interventions directed at reducing these impact variables, such as modifying tibial shock or step frequency, may decrease the incidence and recurrence of this serious injury.
CPT Jamie B. Morris, DPT, OCS, CSCS, is a fellow of the Keller Army Community Hospital Division I Sports Physical Therapy Fellowship at the United States Military Academy in West Point, NY. LTC Donald L. Goss, PT, PhD, OCS, ATC, is director of the Keller Army Community Hospital Division I Sports Physical Therapy Fellowship at the United States Military Academy.
- Pepper M, Akuthota V, McCarty EC. The pathophysiology of stress fractures. Clin Sports Med 2006;25(1):1-16.
- Rauh MJ, Macera C A, Trone DW, et al. Epidemiology of stress fracture and lower-extremity overuse injury in female recruits. Med Sci Sports Exerc 2006;38(9):1571-1577.
- Taunton JE, Ryan MB, Clement DB, et al. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med 2002;36(2):95-101.
- Matheson GO, Clement DB, McKenzie DC, et al. Stress fractures in athletes. A study of 320 cases. Am J Sports Med 1987;15(1):46-58.
- Coyle EF, Martin WH, Sinacore DR, et al. Time course of loss of adaptations after stopping prolonged intense endurance training. J Appl Physiol 1984;57(6):1857-1864.
- Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech 2011;26(1):78-83.
- Warden SJ, Davis IS, Fredericson M. Management and prevention of bone stress injuries in long-distance runners. J Orthop Sports Phys Ther 2014;44(10):749-765.
- Jones BH, Harris JM, Vinh TN, Rubin C. Exercise-induced stress fractures and stress reactions of bone: epidemiology, etiology, and classification. Exerc Sport Sci Rev 1989;17:379-422.
- Bennell KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in track and field athletes. A twelve-month prospective study. Am J Sports Med 1996;24(6):810-818.
- Kelsey JL, Bachrach LK, Procter-Gray E, et al. Risk factors for stress fracture among young female cross-country runners. Med Sci Sports Exerc 2007;39(9):1457-1463.
- Arendt E, Agel J, Heikes C, Griffiths H. Stress injuries to bone in college athletes: a retrospective review of experience at a single institution. Am J Sports Med 2003:31(6):959-968.
- Scully TJ, Besterman G. Stress fracture–a preventable training injury. Mil Med 1982;147(4):285-287.
- Cosman F, Ruffing J, Zion M, et al. Determinants of stress fracture risk in United States Military Academy cadets. Bone 2013;55(2):359-366.
- Milgrom C, Giladi M, Simkin et al. An analysis of the biomechanical mechanism of tibial stress fractures among Israeli infantry recruits. A prospective study. Clin Orthop 1988;(231):216-221.
- Brudvig TJ, Gudger TD, Obermeyer L. Stress fractures in 295 trainees: a one-year study of incidence as related to age, sex, and race. Mil Med 1983;148(8):666-667.
- Gardner LI, Dziados JE, Jones BH, et al. Prevention of lower extremity stress fractures: a controlled trial of a shock absorbent insole. Am J Public Health 1988;78(12):1563-1567.
- Zatsiorsky VM. Kinetics of Human Motion. Champaign, IL: Human Kinetics; 2002.
- Bennell K, Crossley K, Jayarajan J, et al. Ground reaction forces and bone parameters in females with tibial stress fracture. Med Sci Sports Exerc 2004;36(3):397-404.
- Milner CE, Davis IS, Hamill J. Free moment as a predictor of tibial stress fracture in distance runners. J. Biomech 2006;39(15):2819-2825.
- Milner CE, Ferber R, Pollard CD, et al. Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc 2006;38(2):323-328.
- Pohl MB, Mullineaux DR, Milner CE, et al. Biomechanical predictors of retrospective tibial stress fractures in runners. J Biomech 2008;41(6):1160-1165.
- Davis IS, Milner CE, Hamill J. Does increased loading during running lead to tibial stress fractures? A prospective study. Med Sci Sports Exerc 2004:36(5):S58.
- Cameron KL, Peck KY, Owens BD, et al. Kinematic risk factors for lower-extremity stress fracture injuries. Presented at the Annual Meeting of the American Academy of Orthopaedic Surgeons, Chicago, March 2013.
- Brukner P, Khan K. Brukner & Khan’s Clinical Sports Medicine. Australia: McGraw-Hill Education; 2012.
- Kiuru MJ, Pihlajamaki HK, Hietanen HJ, Ahovuo JA. MR imaging, bone scintigraphy, and radiography in bone stress injuries of the pelvis and the lower extremity. Acta Radiol 2002;43(2):207-212.
- Gaeta M, Minutoli F, Scribano E, et al. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology 2005;235(2):553-561.
- Clansey AC, Hanlon M, Wallace ES, et al. Influence of tibial shock feedback training on impact loading and running economy. Med Sci Sports Exerc 2014;46(5):973-981.
- Willy RW, Buchenic L, Rogacki K, et al. In-field gait retraining and mobile monitoring to address running biomechanics associated with tibial stress fracture: In-field gait retraining and monitoring. Scand J Med Sci Sports 2015 Feb 4. [Epub ahead of print]







Trackbacks/Pingbacks