 By J. Craig Garrison, PhD, PT, ATC, SCS
By J. Craig Garrison, PhD, PT, ATC, SCS
A protocol that includes isolated hip strengthening exercises during the early stages of postoperative rehabilitation after anterior cruciate ligament reconstruction may provide a platform on which to build in the later stages of rehab and may predict future performance.
Injuries to the anterior cruciate ligament (ACL) are common across a variety of sports and are often noncontact in nature. Noncontact ACL injuries typically are associated with sports that involve activities such as cutting, landing, and deceleration.1-4 The mechanism of injury often involves abnormal movement in the frontal and transverse planes of motion, which puts the knee in a position of relative valgus and internal rotation and, in turn, increases strain on the ACL.5-7 Valgus loading of the ACL occurs rapidly following ground contact, and researchers have suggested that weakness8 and poor neuromuscular control1 of the hip musculature contribute to increased loading.
Several other studies have expanded our understanding of the relationship between hip strength and lower extremity mechanics. A study of 30 healthy individuals established a relationship between hip strength and valgus movement during a single-leg squat.9 Those with less hip abduction strength demonstrated greater knee movement in a valgus direction during the single-leg squat than individuals with greater hip strength. Similarly, Willson et al found hip external rotation strength was associated with frontal plane knee motion during a single-leg squat in a population of college athletes.10 And Jacobs et al reported that, during a single limb landing maneuver, women (who have a higher risk of ACL injury than their male counterparts11) demonstrated decreased peak hip abductor torque and increased knee valgus compared with men.12
[wc_testimonial position=”left”]Preoperative risk factors involving hip strength, biomechanics, and neuromuscular control may still persist following primary anterior cruciate ligament reconstruction.[/wc_testimonial]
Homan et al found that, when a double-limb landing task was performed, healthy active individuals contacted the ground with slight knee valgus that increased during the loading phase of the landing.13 When the researchers examined these landing kinematics for isometric hip abductor and external rotation strength, they found no differences between the high- and low-strength groups. However, those with lower hip strength values demonstrated greater muscle activity in the gluteus medius and maximus during the landing, indicating a possible increase in neural drive.13
These results suggest that hip strength and neuromuscular control are related to altered positioning of the knee and may play a role in the risk of ACL injury. This is consistent with the findings of Leetun et al, who tracked lower extremity injuries in college athletes and found that those who did not sustain a lower extremity injury during a season had greater hip abduction and external rotator strength than those who were injured.14
 Hip strength and prevention
Hip strength and prevention
Although the literature suggests that decreased hip strength can lead to biomechanical alterations that are associated with ACL injury risk, there is limited evidence to support hip strengthening either for prevention of primary ACL injury or following ACL reconstruction (ACLR) to prevent reinjury. In a hip-focused training program of healthy women aged between 18 and 25 years, investigators saw significant improvements in landing kinematics after the training, signifying a potential model for ACL prevention.15 Following four weeks of plyometric and balance exercises with an emphasis on the hip, maximal isometric strength of the hip abductors and hip extensors increased, and the participants utilized greater hip and knee flexion and lower knee abduction (valgus) angles during landing. Although this study was performed in a healthy population, and the effects of the program were not tracked for future ACL tears,15 the results do suggest the potential for effectively reducing ACL injury risk.
The majority of evidence linking hip strength and knee pain has previously been established in the patellofemoral pain (PFP) literature.16-18 However, increasing numbers of studies have suggested that multiple biomechanical variables, including knee valgus angle and hip muscle weakness, appear to be risk factors for both ACL injury and PFP.1,19-24 Because of these apparent mechanistic similarities between ACL injury and PFP, studies that have reported improvements in pain, knee kinematics, and outcome scores in patients with PFP following a course of hip abductor, extensor, and external rotator strengthening exercises16,17,25,26 may suggest that this treatment also would be beneficial in those who have undergone ACLR.
Our research
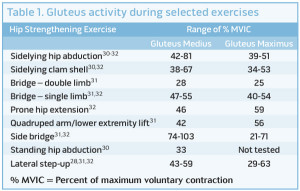
A recent study by this author and colleagues compared the effects of hip strengthening versus no hip strengthening on early outcomes following ACLR.27 Forty-three participants (21 women) volunteered for a study to assess the effect of adding hip strengthening to standard rehabilitation for 12 weeks after ACLR. Patients were randomly enrolled into either a group that performed traditional ACL rehabilitation plus the addition of isolated hip strengthening exercises (Hip group) or traditional ACL rehabilitation alone (NoHip group). The Hip group performed hip strengthening exercises two times per week during the first eight weeks of rehabilitation following ACLR, while those in the NoHip group were not allowed to perform any hip strengthening exercises during the first eight weeks. The hip strengthening exercises (Table 1) performed during this study have been shown to elicit a strength training stimulus in the gluteus medius and gluteus maximus muscles of a healthy population.28-32
Knee extension range of motion (ROM), pain, and Y Balance Test-Lower Quarter (YBT-LQ) performance were assessed at eight and 12 weeks postoperatively. While no significant differences were seen between groups at eight weeks for ROM, pain, or YBT-LQ, significant (p = .008) side-to-side limb differences (involved to uninvolved) in the YBT-LQ anterior reach were found between groups at 12 weeks.27 Hip group participants demonstrated significantly smaller side-to-side limb differences in the YBT-LQ anterior reach (2.7 ± 2.9 cm) than those in the NoHip group (6.1 ± 4.6 cm). We attributed these between-group differences for single-limb activities to possible improvements in hip strength,27 improvements in proximal neuromuscular control at the hip and trunk, or both.31 (The study did not measure hip strength.)
Previously, the anterior reach of the YBT-LQ has demonstrated a higher normalized electromyography (EMG) signal in the gluteus medius than the posteromedial reach.32 Likewise, the anterior reach is essentially a single-leg squat and therefore produces high EMG activation of the gluteus medius and maximus,29,32 as well as earlier gluteus medius activity in those who produce a “good” squat.34 This increase in gluteal activation during the single-leg squat is believed to minimize trunk collapse and valgus movement at the knee.34
Because knee valgus loading and compensations at the contralateral hip/trunk have been implicated in contributing to a second ACL injury,35 a rehabilitation program that addresses altered hip and knee kinematics through the use of hip strengthening exercises appears to be important.27 Additionally, our findings27 suggest that hip strengthening exercises performed in the early stages of rehabilitation following ACLR may provide a platform on which to build in the later stages of the rehabilitation and return-to-sport processes.

Figure 1. If the goal is to minimize valgus movement of the knee during a squat, a resistance band can be placed around the knees and the patient can be instructed to maintain tension of the band during the squat.
Neuromuscular control
The data to support hip strengthening to improve patient outcomes following ACLR are unfortunately sparse. However, new evidence suggests that preoperative risk factors of decreased neuromuscular control and altered biomechanics in the lower extremity may still persist following primary ACLR.35,36 Of 56 athletes who completed a biomechanical screening following primary ACLR, 13 suffered a subsequent ACL tear. Predictors of ACL injury in this group of individuals included altered neuromuscular control at the hip and knee during landing, as well as decreased single-limb postural stability.35
In another study, a group of 78 patients (mean age, 17.1 ± 3.1 years) who had undergone primary ACLR and had returned to sports were prospectively followed and compared with 47 controls with no history of ACL injury (mean age, 17.2 ± 2.6 years) for up to two years after returning to their respective sports. The overall incidence of a second ACL injury was approximately six times higher in the group with a previous ACLR than in the healthy group.36 Some of the factors that could have potentially persisted in the group with a history of ACLR included increased knee valgus and altered hip kinematics during dynamic athletic activities,1,3,37 which may be related to deficits in strength and neuromuscular control at the hip.35 Similarly, a deficit in uninvolved net hip external rotation torque during the initial portion of landing has been shown to predict a second ACL injury with high specificity.35
These results suggest that interventions that focus on impairments in both strength and neuromuscular control at the hip could potentially decrease the risk of second ACL injury after ACLR. Therefore, treatment and rehabilitation programs following ACLR should involve exercises that incorporate the hip extensor and external rotator muscles to minimize knee loading in the frontal plane.35
In addition to implementing hip strengthening exercises as part of the post-ACLR rehabilitation program, it may also be beneficial to use neuromuscular training and feedback techniques. Even if patients have undergone a hip strengthening program and developed increased strength, they don’t necessarily improve the functional use of that new strength. Gokeler et al have proposed incorporating feedback training that utilizes an external focus for optimization of training adaptations following ACLR.38 Using an external focus training technique directs the patient’s attention to the effects of the movement being performed or to the overall outcome of the movement rather than to the movement itself. For example, if the goal is to minimize valgus movement of the knee during a squat, a resistance band can be placed around the knees and the patient can be instructed to maintain tension of the band during the squat (Figure 1).

Figure 2. If frontal plane knee alignment during jump landing is the goal of training, pieces of tape can be placed on the floor and the patella (top image), and the patient instructed to keep the two sets of tape in alignment during the landing movement (bottom image).
In a study of 28 healthy recreational athletes performing a landing task, a resistance band placed around the ankles effectively increased the internal hip abductor moment (hip abductor muscle force) and gluteus muscle EMG activity during prelanding and early landing.39 These results support the idea that the application of a resistance band around the lower extremities may provide a training strategy for hip abductor strength and activation during dynamic
activities.
Additionally, if frontal plane knee alignment during jump landing is the goal of training, pieces of tape may be placed on the floor and the patella, and the patient instructed to keep the two sets of tape in alignment during the landing movement (Figure 2). This type of training promotes motor learning and the effective use of automatic processing or unconscious control.40 Likewise, the patient can learn to use the newly developed hip strength, which may help to improve function and decrease risk of reinjury to the knee.
In a related study, 12 female Division I soccer players completed a 10-week augmented feedback neuromuscular training program and demonstrated improved hip and knee mechanics (decreased knee valgus) during a stop-jump task, as well as increased isometric hip extension strength.41 The results reinforce the importance of feedback in relation to quality and efficiency of movement as a means of both improving performance and preventing injury.
Conclusion
Although the data in the literature supporting hip strengthening following ACLR are limited at this time, emerging evidence suggests a protocol that includes isolated hip strengthening exercises during the early stages of postoperative rehabilitation can improve single-limb balance and neuromuscular control at the three-month mark.27 These improvements demonstrated during a single-limb squat may provide a platform on which to build in the later stages of postoperative ACL rehabilitation and may predict future performance on functional hop tests at the time of return to sport.42
Similarly, once hip strength has been established following ACLR, feedback and technique training using an external focus38 may be important for the functional implementation of the hip strength development during dynamic movement tasks that must be mastered prior to returning to sport.
The fact that altered hip and knee kinematics are among the potential biomechanical and neuromuscular risk factors for injury to the ACL1,35,36 suggests that hip strength may play a role in the mechanism of injury and reinjury. Therefore, there is a need for continued research that examines the effects of hip strengthening following ACLR, particularly the potential benefits that may be seen at the time of return to sport.
Craig Garrison, PhD, PT, ATC, SCS, is director of research and professional development at the Texas Health Ben Hogan Sports Medicine, adjunct assistant professor in the Physical Therapy Program at the University of North Texas Health Science Center, and adjunct assistant professor in the Department of Kinesiology, Harris College of Nursing and Health Sciences, at Texas Christian University, all in Fort Worth.
- Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes. Am J Sports Med 2005;33(4):492-501.
- Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries. Knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med 2010;38(11):2218-2225.
- Krosshaug T, Slauterbeck JR, Engebretsen L, Bahr R. Biomechanical analysis of anterior cruciate ligament injury mechanisms: three-dimensional motion reconstruction from video sequences. Scand J Med Sci Sports 2007;17(5):508-519.
- Joseph MF, Rahl M, Sheehan J, et al. Timing of lower extremity frontal plane motion differs between female and male athletes during a landing task. Am J Sports Med 2011;39(7):1517-1521.
- Markolf KL, Burchfield DM, Shapiro MM, et al. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res 1995;13(6):930-935.
- Quatman CE, Kiapour AM, Demetropoulos CK, et al. Preferential loading of the ACL compared with the MCL during landing. A novel In Sim approach yields the multiplanar mechanism of dynamic valgus during ACL injuries. Am J Sports Med 2013;42(1):177-186.
- Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball. A systematic video analysis. Am J Sports Med 2004;32(4):1002-1012.
- Geiser CF, O’Connor KM, Earl JE. Effects of isolated hip abductor fatigue on frontal plane knee mechanics. Med Sci Sports Med 2010;42(3):535-545.
- Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech 2006;22(1):41-50.
- Willson JD, Ireland ML, Davis IS. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Med 2006;38(5):945-952.
- Hutchinson MR, Ireland ML. Knee injuries in female athletes. Sports Med 1995;19(4):288-302.
- Jacobs CA, Uhl TL, Mattacola CG, et al. Hip abductor function and lower extremity landing kinematics: sex differences. J Athl Train 2007;42(1):76-83.
- Homan KJ, Norcross MF, Goerger BM, et al. The influence of hip strength on gluteal activity and lower extremity kinematics. J Electromyogr Kinesiol 2013;23(2):411-415.
- Leetun DT, Ireland ML, Willson JD, et al. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc 2004;36(6):926-934.
- Stearns KM, Powers CM. Improvements in hip muscle performance result in increased use of the hip extensors and abductors during a landing task. Am J Sports Med 2014;42(3):602-609.
- Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med 2011;39(1):154-163.
- Fukuda TY, Rossetto FM, Magalhaes E, et al. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther 2010;40(11):736-742.
- Bolgla LA, Malone TR, Umberger BR, Uhl TL. Comparison of hip and knee strength and neuromuscular activity in subjects with and without patellofemoral pain syndrome. Int J Sports Phys Ther 2011;6(4):285-296.
- Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther 2009;39(1):12-19.
- Boling MC, Padua DA, Marshall SW, et al. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med 2009;37(11):2108-2116.
- Souza RB, Powers CM. Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med 2009;37(3):579-587.
- Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther 2012;42(2):81-94.
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther 2003;33(11):639-646.
- Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med 2008;27(3):425-448.
- Dolak KL, Silkman C, Medina McKeon J, et al. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: a randomized clinical trial. J Orthop Sports Phys Ther 2011;41(8):560-570.
- Ferber R, Kendall KD, Farr L. Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome. J Athl Train 2011;46(2):142-149.
- Garrison JC, Bothwell J, Cohen K, Conway JE. Effects of hip strengthening on early outcomes following anterior cruciate ligament reconstruction. Int J Sports Phys Ther 2014;9(2):157-167.
- Ayotte NW, Stetts DM, Keenan G, Greenway EH. Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight-bearing exercises. J Orthop Sports Phys Ther 2007;37(2):48-55.
- Distefano LJ, Blackburn JT, Marshall SW, Padua DA. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther 2009;39(7):532-540.
- Bolgla LA, Uhl TL. Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects. J Orthop Sports Phys Ther 2005;35(8):487-494.
- Ekstrom RA, Donatelli RA, Carp KC. Electromyographic analysis of core, trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther 2007;37(12):754-762.
- Boren KB, Conrey C, Le Coguic J, et al. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther 2011;6(3):206-223.
- Norris B, Trudelle-Jackson E. Hip and thigh muscle activation during the Star Excursion Balance Test. J Sport Rehabil 2011;20(4):428-441.
- Crossley KM, Zhang WJ, Schache AG, et al. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med 2011;39(4):866-873.
- Paterno MV, Schmitt LC, Ford KR, Rauh MJ. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38(10):1968-1978.
- Paterno MV, Rauh MJ, Schmitt LC, et al. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med 2014;42(7):1567-1573.
- McClean SG, Huang X, van den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech 2005;20(8):863-870.
- Gokeler A, Benjaminse A, Hewett TE, et al. Feedback techniques to target functional deficits following anterior cruciate ligament reconstruction: implications for motor control and reduction of second injury risk. Sports Med 2013;43(11):1065-1074.
- Dai B, Heinbaugh EM, Ning X, Zhu Q. A resistance band increased internal hip abduction moments and gluteus medius activation during pre-landing and early-landing. J Biomech 2014;47(15):3674-3680.
- Wulf G, McNevin N, Shea CH. The automaticity of complex motor skill learning as a function of attentional focus. Q J Exp Psychol A 2001;54(4):1143-1154.
- Greska EK, Cortes N, Van Lunen BL, Onate JA. A feedback inclusive neuromuscular training program alters frontal plane kinematics. J Strength Cond Res 2012;26(6):1609-1619.
- Garrison JC, Bothwell J, Wolf G, et al. Single leg squat symmetry at 3 months is related to single leg functional performance at time of return to sports following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther [In Press].








