The medical literature doesn’t yet have all the answers regarding orthotic management of stroke, but don’t discount the existing body of evidence. It could—and should—change the way you practice.
by Stefania Fatone, PhD, BPO(Hons)
The orthotic management of stroke has garnered much interest recently, due in part to the growing number of persons rehabilitating from stroke and the push for evidence-based practice in orthotics. According to data compiled by the American Heart Association,1 each year about 610,000 people experience a first stroke and 185,000 have a recurrent attack. Although stroke affects persons of all ages, it is largely a disease of the elderly, and the number of Americans aged 65 and over is increasing.2 This growth in the number of elderly people means that the total number of strokes is expected to increase by 20% in 2010 and more than double by 2050.3
A stroke typically results in hemiparesis or hemiplegia, wherein one side of the body is weakened or paralyzed. Stroke is a leading cause of serious, long-term disability in the United States with 15% to 30% of stroke survivors left permanently disabled, and 20% requiring institutional care at three months after onset.1 In 1999, more than 1.1 million American adults reported difficulty with functional activities and activities of daily living resulting from stroke.4 Among stroke survivors who were at least 65 years of age, 50% had some hemiparesis, 30% were unable to walk without some assistance, and 26% were dependent in activities of daily living six months after stroke.1
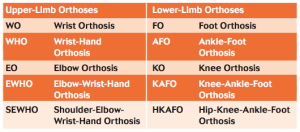
An orthosis is defined by the International Standards Organization5 as “an externally applied device used to modify the structural and functional characteristics of the neuromuscular and skeletal system.” Orthoses can be fitted to almost any part of the body from the leg to the arm, spine, and head. Standardized nomenclature and a system of acronyms are used to identify different orthotic devices based on the principal joints the orthosis encompasses and is intended to control or effect.6 This system forms the core of the ISO 8549-3 general descriptors for orthoses.7 Table 1 provides the nomenclature system for upper- and lower-limb orthoses that might be used by persons with stroke.
The Push for Evidence
The push for evidence based practice extends to all areas of health care, including orthotics. According to the Center for Evidence Based Medicine (EBM) at the University of Toronto, “Evidence-based medicine [or practice] is the integration of best research evidence with clinical expertise and patient values.” This approach to patient care requires that clinicians consult and apply the best available research evidence to the care of individual patients.8 However, the results of individual studies cannot be interpreted with any confidence unless they have been considered, systematically, together with the results of other studies addressing the same or similar questions. Hence, systematic reviews are undertaken to provide an overview of primary studies that have been conducted according to explicit and reproducible methodology.
Equinovarus positioning of the ankle-foot complex is the most common deformity observed in the lower-limb following stroke,9 hence ankle-foot orthoses (AFOs) are the most commonly prescribed orthosis for management of gait abnormalities following stroke.10 AFOs, which encompass the ankle joint and the whole or part of the foot,11 are intended to control motion, correct deformity, and/or compensate for weakness.12 They can be designed with sufficient mechanical lever arms to control the ankle-foot complex directly and to influence the knee joint indirectly,12 especially where the knee is unstable or a hyperextension deformity has developed. AFOs are presently the type of orthosis most frequently prescribed by certified orthotists in the United States, accounting for 26% of clinical practice—double that of any other type of orthosis.13 Although there are many types of AFOs, which vary in their biomechanical design, materials and components, they can be rationally prescribed based on their biomechanical function.14
AFO designs fall into two main categories: articulated and non-articulated.10 As the name implies, articulated AFOs incorporate mechanical joints at the ankle and may be used to control joint range of motion (e.g., using adjustable joints), provide assistance to motion (e.g., with a dorsiflexion assist joint), or limit motion (e.g., with plantar flexion or dorsiflexion stops). Although non-articulated AFOs do not incorporate joints, they may or may not allow motion at the ankle in the sagittal plane, depending on their flexibility. In a non-articulated polymer or thermoset AFO, motion is determined by the rigidity of the orthosis about the ankle joint, which is usually a product of material thickness, geometry or composition. Adding reinforcements about the ankle or an anterior shell may also increase rigidity of the AFO. A non-articulated AFO is generally rigid if the trim-lines about the ankle are anterior to the malleoli, in which case it is sometimes referred to as a solid or rigid AFO. The more posterior the trim-lines are to the malleoli, the more flexible the orthosis becomes, such as in a polymer posterior leaf spring AFO (PLS-AFO). In a PLS-AFO, motion occurs due to buckling or deformation of the plastic when a moment is applied.
A comprehensive review of the orthotic management of stroke was undertaken by the International Society for Prosthetics and Orthotics (ISPO) in 2003 as part of a multidisciplinary consensus conference.14 A number of reviews specific to AFOs were conducted as part of this conference: Campbell15 reviewed 21 articles demonstrating attempts made to ground orthotic management in evidence, Bowers16 reviewed 21 articles related specifically to efficacy of non-articulated AFOs in persons with stroke, and Hoy and Reinthal17 reviewed 18 articles related specifically to efficacy of articulated AFOs in persons with stroke.
Evidence-based recommendations
Based on these reviews and consensus of the multidisciplinary experts, ‘best practice points’ were recommended for the lower-limb orthotic management of stroke (Table 2).14 Due to the limited number of unbiased clinical studies regarding the effectiveness of orthotic intervention for stroke,18 most of the recommended ‘best practice points’ were based upon the clinical experience of the consensus conference attendees.14 Similarly, a number of other organizations have made recommendations regarding orthotic management of stroke, in particular the use of AFOs,19-22 with the general consensus that AFOs should be considered for people with foot drop and that they should be individually fitted, particularly once long-term need is established.
Three systematic reviews regarding the effect of AFOs on the management of persons with stroke have been published more recently.23-25 Van Peppen et al24 reviewed the impact of physical therapy on functional outcomes after stroke, including the application of AFOs, limiting the search to randomized controlled or controlled clinical trials. Only one randomized clinical trial (RCT) that investigated the effect of an AFO on walking ability and gait speed was identified and reviewed.26 Based solely on this RCT, Van Peppen et al24 concluded that there was no evidence for increased gait speed when an AFO was provided after stroke.
Using broader criteria for study selection, Leung and Moseley23 reviewed the impact of AFOs on gait and lower-limb muscle activity in adults with hemiplegia. This review included 13 studies on gait and four on muscle activity, all of which were either cross-over (n=9) or single case studies (n=4). In contrast to the review by Van Peppen et al,24 Leung and Moseley23 excluded the RCT by Beckerman et al26 due to methodological problems such as poor compliance with the orthotic regimen in about half of patients, problems with fit of the AFOs in more than 67% of patients, and use of a “placebo AFO” as a control rather than comparison to a without-AFO condition. Leung and Moseley23 concluded that AFOs might improve velocity, stride length, gait pattern and walking for people with hemiplegia, but that the effect of AFOs on paretic lower-limb muscle activity was inconclusive.
A Cochrane systematic review by Tyson and Kent25 attempted to determine the effectiveness of upper- or lower-limb orthoses on activity and impairment in people with stroke and other nonprogressive brain lesions. With regard to lower-limb orthoses, they concluded that the overall effect of AFOs on walking disability (speed), walking impairment (step/stride length) and balance impairment (weight distribution in standing) was significant and beneficial based on 14 cross-over trials that looked at the immediate effect of wearing an orthosis. The orthoses used in the studies reviewed by Tyson and Kent24 demonstrate the range of clinically prescribed orthoses for stroke patients: typically custom-made thermoplastic, posterior shell designs that extend to the toes and are either rigid or articulated with a posterior plantar flexion stop. Although pre-fabricated thermoplastic posterior leaf spring AFOs have been assessed for use by persons with post-stroke hemiplegia, they are not recommended where spasticity is present since they provide insufficient resistance and control of ankle-foot equinovarus posturing.14
Communicating the Evidence
More recently the need for diverse forms of research dissemination have been acknowledged as part of the broader concept of knowledge translation.27 Knowledge translation has been defined by the National Center for Dissemination of Disability Research as “the collaborative and systematic review, assessment, identification, aggregation and practical application of high-quality disability and rehabilitation research by key stakeholders (i.e., consumers, researchers, practitioners, policy makers) for the purpose of improving the lives of individuals with disabilities.”28 In contrast, ‘research dissemination’ has the more narrow connotation of spreading knowledge or research through scientific journals and at scientific conferences.27
It has been acknowledged that a gap exists between those who produce research and those who must ultimately apply it to improve the lives of persons with disability29, 30 leading to ineffective communication of research findings31-33 and a perceived lack of timeliness and relevance of the research findings by clinicians.29,30, 34 Furthermore, clinicians often lack the time and critical appraisal skills required to review and synthesize complex research findings.31,35,36 Hence, different dissemination approaches are needed to effectively communicate research findings to different stakeholders.36-38 The American Academy of Orthotists & Prosthetists (AAOP) and the American Orthotic & Prosthetic Association have engaged in activities aimed at facilitating knowledge translation, including providing a continuing education course on this topic (Certificate Course on Orthotic Management of the CVA/Stroke Patient) and sponsoring the publication and dissemination of an Evidence Note on the use of AFOs in the management of stroke.39 An evidence note provides a brief, plain language summary of the available evidence on a particular topic and typically involves systematic appraisal of the most up-to-date secondary literature.40 The evidence note on the use of ankle foot orthoses in the management of stroke39 provides a condensed four page summary of some of the material included in the 273-page ISPO consensus conference report.14 Both of these documents may be freely accessed on line (Table 3). Similarly, publications such as Lower Extremity Review provide another important forum for disseminating research findings to a wider audience.
These various syntheses of the literature provide evidence that AFOs should be considered in the management of stroke by providing important evidence of the efficacy of these devices for that patient population. However, the evidence remains at an insufficient level to fully inform clinical practice, and many crucial questions remain unanswered. Clinicians still need to know the best type of orthosis to prescribe, for whom they should be prescribed, the optimal time to prescribe an AFO, how long they should be used, the adverse effects, and the factors influencing acceptability and adherence to their use.25 It is particularly important that these factors are investigated in the long term, as most patients are prescribed an AFO for long-term use. Additionally, it has been recommended by the ISPO consensus conference on Orthotic Management of Stroke Patients14 that advances in future research will require agreed-upon standards of terminology and definitions; clearly defined biomechanical design, materials and components of the orthoses; and well-controlled, multidisciplinary, multicenter research. It was further suggested that the ‘good practice points’ recommended in the ISPO report should be used as a basis for research priorities.14
Although it is clear that we need additional research regarding lower-limb orthotic management of stroke, we should not delay implementing the evidence that we have, for it is possible to use the best available evidence as it currently exists to inform clinical practice and in so doing improve the quality of patient care.
Stefania Fatone, PhD, BPO(Hons), is a research assistant professor in the Northwestern University Feinberg School of Medicine’s department of physical medicine and rehabilitation, and the Northwestern University Prosthetics Research Laboratory and Rehabilitation Engineering Research Program, both in Chicago IL.
The author does not declare any financial conflict of interest.
Table 1. A selection of general descriptors for lower-limb orthoses as defined by ISO 8549-37
Table 2. Best practice points as recommended in the ISPO Consensus Conference Report on Orthotic Management of the Stroke Patient14,41
Table 3. Additional Resources
Evidence Note: The Use of Ankle Foot Orthoses in the Management of Stroke
ISPO Report of a consensus conference on the orthotic management of stroke patients
References
1. Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics – 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119(3):480-486.
2. U.S. Department of Health and Human Services Administration on Aging. A statistical profile of older americans aged 65+. Snapshot, U.S. Department of Health and Human Services Administration on Aging, Washington, D.C. 2008.
3. Olsen T. Stroke – Understanding the problem. In: Condie E, Campbell J, Martina J, eds. Report of a Consensus Conference on the Orthotic Management of Stroke Patients. 1st ed. Copenhagen, Denmark: International Society for Prosthetics and Orthotics; 2004:37-44.
4. Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics – 2008 update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008;117(4):e1-e128.
5. International Organization for Standardization. ISO 8549-1:1989 Prosthetics and Orthotics – Vocabulary. General terms for external limb prostheses and orthoses. Geneva, Switzerland: International Organization for Standardization; 1989.
6. Harris EE. A new orthotics terminology: a guide to its use for prescription and fee schedules. Orthot Prosthet 1973;27(2):6-19.
7. Condie DN. International Organization for Standardization (ISO) Terminology. In: Hsu JD, Michael JW, Fisk JR, eds. AAOS Atlas of Orthoses and Assistive Devices. 4th ed. Philadelphia, PA: Mosby Elsevier; 2008:3-7.
8. Sackett DL, Rosenberg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn’t. BMJ 1996;312(7023):71-72.
9. Fennell CW, Yang AN, Elson D. Orthoses for brain-injured patients. In: Goldberg B, Hsu J, eds. Atlas of Orthoses and Assistive Devices. 3rd ed. St Louis, MO: Mosby; 1997:379-389.
10. Fatone S. Ch. 31. Orthotic Management in Stroke. In: Stein J, Harvey RL, Macko RF, et al, eds. Stroke Recovery and Rehabilitation. 1st ed. New York: Demos Medical Publishing; 2008:515-530.
11. International Organization for Standardization. ISO 8549-3:1989 Prosthetics and Orthotics – Vocabulary. Terms relating to external orthoses. Geneva, Switzerland: International Organization for Standardization; 1989.
12. Michael JW. Lower limb orthoses. In: Hsu JD, Michael JW, Fisk JR, eds. AAOS Atlas of Orthoses and Assistive Devices. 4th ed. Philadelphia, PA: Mosby Elsevier; 2008:343-355.
13. Whiteside SR, Allen MJ, Barringer WJ, et al. Practice analysis of certified practitioners in the disciplines of orthotics and prosthetics. Alexandria, VA: American Board for Certification in Orthotics and Prosthetics, Inc.; 2007.
14. Condie E, Campbell J, Martina J, eds. Report of a Consensus Conference on the Orthotic Management of Stroke Patients. 1st ed. Copenhagen, Denmark: International Society for Prosthetics and Orthotics; 2004.
15. Campbell J. Establishing a scientific basis for orthotic management. In: Condie E, Campbell J, Martina J, eds. Report of a Consensus Conference on the Orthotic Management of Stroke Patients. 1st ed. Copenhagen, Denmark: International Society for Prosthetics and Orthotics; 2004:83-86.
16. Bowers RJ. Non-articulated ankle-foot orthoses. In: Condie E, Campbell J, Martina J, eds. Report of a Consensus Conference on the Orthotic Management of Stroke Patients. 1st ed. Copenhagen, Denmark: International Society for Prosthetics and Orthotics; 2004:87-94.
17. Hoy DJ, Reinthal MA. Articulated ankle foot orthoses designs. In: Condie E, Campbell J, Martina J, eds. Report of a Consensus Conference on the Orthotic Management of Stroke Patients. 1st ed. Copenhagen, Denmark: International Society for Prosthetics and Orthotics; 2004:95-111.
18. Morris C. Current research in orthotics. In: Condie E, Campbell J, Martina J, eds. Report of a Consensus Conference on the Orthotic Management of Stroke Patients. 1st ed. Copenhagen, Denmark: International Society for Prosthetics and Orthotics; 2004:269-273.
19. VA/DoD. VA/DoD Clinical practice guideline for the management of stroke rehabilitation. VA Employee Education System in cooperation with the Offices of Quality & Performance and Patient Care Services and the Department of Defense; 2002.
20. Scottish Intercollegiate Guidelines Network (SIGN). Management of patients with stroke: rehabilitation, prevention and management of complications, and discharging planning; a national clinical guideline. Edinburgh, Scotland: Scottish Intercollegiate Guidelines Network; 2002.
21. National Stroke Foundation. Clinical guidelines for stroke rehabilitation and recovery. National Stroke Foundation. Approved by National Health and Medical Research Council, Australian Government; 2005.
22. Royal College of Physicians. National clinical guidelines for stroke. Second edition. London: Royal College of Physicians of London. Prepared by the Intercollegiate Stroke Working Party; 2004.
23. Leung J, Moseley AM. Impact of ankle-foot orthoses on gait and leg muscle activity in adults with hemiplegia. Physiotherapy 2003;89(1):39-55.
24. van Peppen RP, Kwakkel G, Wood-Dauphinee S, et al. The impact of physical therapy on functional outcomes after stroke: what’s the evidence? Clin Rehabil 2004;18(8):833-862.
25. Tyson SF, Kent RM. Orthotic devices after stroke and other non-progressive brain lesions. Cochrane Database of Systematic Reviews 2009;(1):CD003694.
26. Beckerman H, Becher J, Lankhorst GJ, Verbeek AL. Walking ability of stroke patients: efficacy of tibial nerve blocking and a polypropylene ankle-foot orthosis. Arch Phys Med Rehabil 1996;77(11):1144-1151.
27. Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: Time for a map? J Contin Educ Health Prof 2006;26(1):13-24.
28. National Center for Dissemination of Disability Research. What is knowledge translation? Focus. National Center for Dissemination of Disability Research; 2005.
29. Farkas M, Anthony WA. Bridging science to service: using Rehabilitation Research and Training Center program to ensure that research-based knowledge makes a difference. J Rehabil Res Dev 2007;44(6):879-892.
30. Jette DU, Bacon K, Batty C, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther 2003;83(9):786–805.
31. Dobbins M, Rosenbaum P, Plews N, et al. Information transfer: what do decision makers want and need from researchers? Implement Sci 2007 Jul 3;2:20.
32. Draper B, Low L-F, Withall A, et al. Translating dementia research into practice. Int Psychogeriatr 2009;21(Suppl 1):S72-S80.
33. Choi BC. Understanding the basic principles of knowledge translation. J Epidemiol Community Health 2005;59(2)93.
34. Kitson AL. The need for systems change: reflections on knowledge translation and organizational change. J Adv Nurs 2009;65(1):217-228.
35. Baumbusch JL, Kirkham SR, Khan KB, et al. Pursuing common agendas: a collaborative model for knowledge translation between research and practice in clinical settings. Res Nurs Health 2008;31(2):130-140.
36. Demers L, Poissant L. Connecting with clinicians: opportunities to strengthen rehabilitation research. Disabil Rehabil 2009;31(2):152-159.
37. Lavis JN, Robertson D, Woodside JM, et al. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q 2003;81(2):221-248.
38. Eastwood GM, O’Connell B, Gardner A. Selecting the right integration of research into practice strategy. J Nurs Care Qual 2008;23(3):258-265.
Fatone S, Campbell J. The use of ankle foot orthoses in the management of stroke. Evidence Note. Alexandra, VA: Orthotic and Prosthetic Outcomes Initiative Steering Committee; 2008.
University of Birmingham. West Midlands Health Technology Assessment Collaboration: Accessed on July 6, 2009.
40. Condie E, Bowers R. Lower limb orthoses for persons who have had a stroke. In: Hsu JD, Michael JW, Fisk JR, eds. AAOS Atlas of Orthoses and Assistive Devices. 4th ed. Philadelphia, PA: Mosby Elsevier; 2008:433-440.
41. Shekelle PG, Woolf SH, Eccles M, Grimshaw J. Clinical guidelines: developing guidelines. Br Med J 1999;318(7183):593-596.