Who is this for?
People suffering with pain from their bunion deformity that aren’t ready for, or cannot have surgical correction.
What is a bunion?
The bunion deformity, technically termed Hallux Abductovalgus or HAV for short, is much more than just a bump of bone growing on the foot. Technically, it is a 3-dimensional positional misalignment of the entire 1st ray, which includes the great toe and the first metatarsal (Figure 1). Simply put, it’s a biomechanical misfit between the bones that control your big toe—but not just in 1 direction or on one plane; the misalignment can occur in any of the 3 planes in which your foot bones normally move—up, down, sideways. Bunions are not caused by ill-fitting shoes, although the wrong shoes can make a bunion more painful. Bunions are usually hereditary, meaning you inherit the foot type that is predisposed to bunion formation. Bunions can appear at any age, but most people begin to notice them in the later teen years. Other causes of bunions are certain traumas and arthritic conditions that disrupt the normal anatomic stabilizing structures. Women may also develop bunions during pregnancy when several body ligaments become more lax (loose).
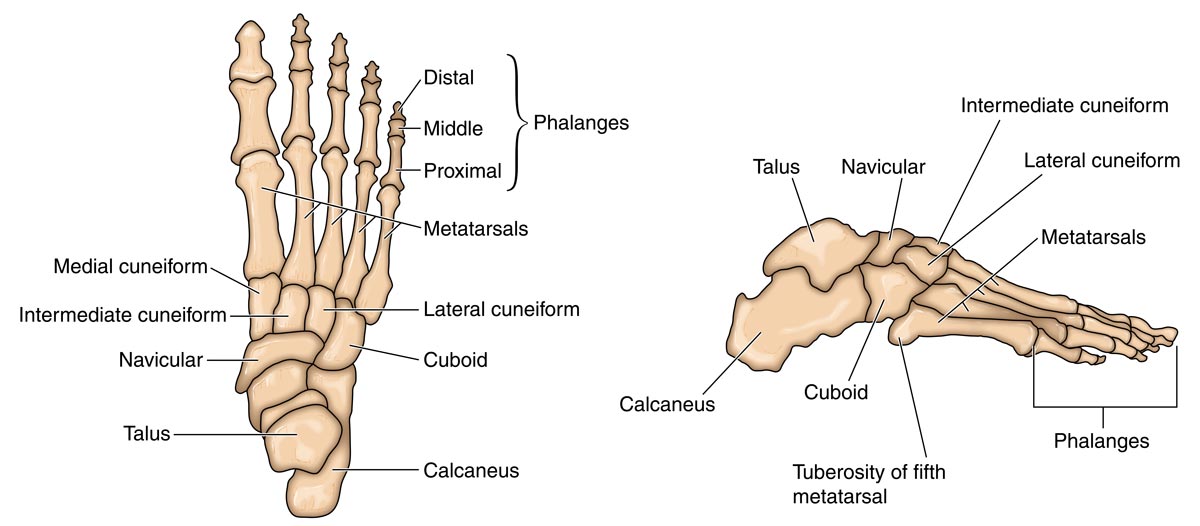
It is thought by most biomechanical experts that the bunion deformity is caused by an unstable 1st ray. This 1st ray instability is often related to rear-foot joint instability, particularly in the sub-talar and mid-tarsal joint complex (Figure 2). Rear-foot instability allows the talus bone to slide out of position, moving forward, downward and medially (toward the inside of your foot). This leads to an excessively pronated position of the foot (pronation is when your ankle moves toward the inside of your foot). In this position, the arch appears to flatten as the foot rolls inward. When this pronated position persists during the gait cycle of walking, when the foot should be returning to the more stable supinated (outward tilting) position, the mechanical effectiveness of the main muscular stabilizer of the first ray, the peroneus longus, is effectively reduced. In other words, this mispositioning of the foot puts the muscle that controls the big toe into a weakened state. This relative weakness combines with inherited joint surface changes and loosened ligaments to allow for 3-plane 1st ray instability.
First-ray stability is important for pain-free efficient walking. The 1st ray should be stabilized against the ground to prepare the foot for toe off (the first step in the walking cycle). With 1st ray instability, the 1st ray gets pushed upward by the force of body weight, making it raised or elevated compared to the other metatarsals. This can allow the foot to turn inward even more, making rear-foot instability worse. With continued stress, the 1st ray will begin to twist into a position of valgus – picture the toe nail of the great toe is not facing straight up, but rather facing the other foot. The 1st metatarsal will begin to move away from the mid-line of the foot and begin to protrude on the medial or inside of the foot. In other words, that 1st metatarsal is now pointing toward the other foot, not straight forward.
Most bunion symptoms begin when this boney spur or prominence starts interacting with footwear. With progression of the deformity, severe joint misalignment can occur, leading to joint damage and arthritis. Bunions progress at different rates for different people. Like most conditions, early intervention can prevent later problems.
Can bunions be prevented?
Although we cannot say that bunions can be prevented, it is my belief and experience of 25 years in treating this condition, that controlling abnormal foot mechanics can not only reduce the symptoms of a bunion, but can also slow down or even halt its progression.
Fun Fact!

Star Trek’s Captain Kirk had bunions!
Well, actually, the actor who played the beloved captain of the Starship Enterprise, William Shatner, has bunions. In his 2018 autobiography, he mentions them:
“When people come to me and ask for advice, assuming I must have learned something vitally important in my lifetime, I respond with the best possible advice: Don’t follow my advice. Each one of us is unique. Different. Not the same. You didn’t have my mother. No one else can walk in my shoes; most people can’t even fit into them. I can’t wear your shoes; they make my bunions pinch. But why try? We each bring to everyday an entirely different set of experiences and a unique personal point of view. We each see life through a different prism. We are physically, emotionally, and mentally different. We think and see and feel the same things differently. The breeze, the sensation of putting oil on my skin, the anger I feel when some driver cuts me off, my response to a joke or a movie — it’s different, all of it.
For me, really for anyone, to try to tell anyone else how to live their life is the ultimate in hubris. There is no one way, or right way, to do anything. Is there only one path up a mountain? Is there only one way to maintain your health? Is there one way to have a relationship, or is it many and varies depending on whose shoes you have on your feet? I don’t have those answers; maybe the holy men on the top of the mountain do. But they’re living on top of a mountain.”
This is an adapted excerpt from “Live Long And…” by William Shatner with David Fisher. Copyright (c) 2018 by the authors.
Abnormal mechanics can be controlled with orthopedic devices such as foot orthoses and braces. One of the most effective ways to address foot mechanical issues is with custom-molded foot orthoses. These devices are made to the shape of a person’s foot by taking a cast, foam impression, or scan to capture an accurate shape. Corrections are then added to the devices based on the biomechanical findings of the foot and ankle specialist. These devices fit in most shoes and can be moved between shoes. Off-the-shelf devices tend to be less effective at controlling foot mechanics due to their materials (usually too soft) and lack of corrective changes customized to a patient’s unique foot structure or shape. Extreme levels of instability may require bracing that extends above the ankle, known as an ankle foot orthosis, or AFO. These are also custom constructed based on a mold of the foot and leg.
Surgical options for stabilizing a hypermobile rear foot are numerous, ranging from minimally invasive joint stabilization to major bone reconstructions and joint fusions. Surgical options will be discussed in the next article.
What about the bunion itself?
Many devices have been designed to attempt to realign the bunion deformity without surgery. Although some may provide a measure of symptom relief, I have yet to find any to be effective in changing the position of the toe on a long-term basis. Conservative care for the bunion involves prevention of symptoms. It starts with ensuring rear-foot stability as discussed earlier. Accommodation of the bunion bump and imperfectly angled toe during shoe wearing is the next step.
Shoes should be wide enough to accommodate the boney prominence. Trace the shape of the foot with a pencil and paper and measure the width at the bunion area. Stretchable upper materials such as Lycra, can be helpful in reducing pressure on the bump. Custom-molded orthopedic shoes are another option if comfort cannot be obtained in conventional or extra depth shoes. There are many padding options available, including foam, gels, rubber, felt, lamb’s wool, and cotton in various shapes and sizes. A foot and ankle specialist or pedorthist can help with these accommodations.
In summary, the bunion deformity, as with many foot and ankle conditions, has abnormal mechanics at the root of the problem. A thorough examination by a foot and ankle specialist is the best way to get the right recommendations for your particular set of circumstances.
Should surgery become necessary, be sure to get more than one opinion from a Board Certified Foot and Ankle Surgeon who is well versed in bunion correction.
Paul J. Betschart, DPM, FACFAS, is a podiatrist in private practice in Danbury, Connecticut. A Fellow of the American College of Foot and Ankle Surgeons, his goal is to help his patients achieve optimal health from the ground up.