istockphoto.com 3633957
Grade 1 and 2 turf toe hyperextension injuries have good outcomes when treated non-operatively. The optimal treatment for grade 3 turf toe injuries with complete capsular avulsion, however, is unclear.
by Seth C. Gamradt, MD, and Robert H. Brophy, MD
“Turf toe” is a term used broadly in sports medicine by health professionals and athletes alike to indicate an injury to the first metatarsophalangeal (MTP) joint. This injury was first described in American football athletes by Bowers and Martin in 1976.1 More specifically, turf toe is a hyperextension injury to the first MTP joint with varying degrees of injury to the plantar capsule, plantar musculature, and sesamoid complex.2 This injury should be differentiated from “sand toe,” which is a hyperflexion injury to the first MTP joint and results in a different spectrum of injury.3
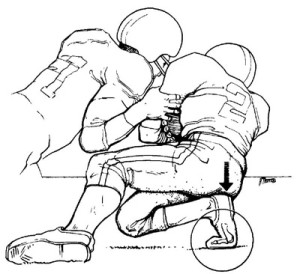
Turf toe is common in American football. The classic description of the injury is depicted in Figure 1 (from Rodeo et al ); a player whose foot is planted on the ground with the heel in the air is subjected to a force on the back of the foot thereby hyperextending the first MTP joint.4 The injury usually happens when a football player’s cleat is engaged with the turf and another player lands on the back of the heel (Figure 1). This brief review outlines the pathoanatomy, classification, imaging, and treatment of turf toe in American football
Epidemiology
In their 1976 article,1 Bowers and Martin described an incidence of 5.4 cases per year during the years 1970-1974 at West Virginia University. At Rice University from 1971 to 1985, the football team averaged 3.8 cases per year, and 84% of these injuries initially occurred on artificial turf.5 At the University of Arkansas from 1972 to 1974, Coker et al6 described an incidence of 6 cases per year on the football team.
The study by Rodeo et al4 was the first to document the prevalence of turf toe among professional football players. They found that 45 % of players (36 of 80) had incurred a turf toe injury at some point in their college or professional career. Of those that recalled the specific injury, 83% reported that the injury had occurred on artificial turf. Older players and those with more experience in professional football were more likely to have sustained a turf toe injury. Rodeo et al were unable to correlate turf toe injury with a particular type of shoe, but did find that athletes sustaining a turf toe injury had a persistent loss of motion at the MTP joint.4
Since these initial epidemiological studies describing the nature and incidence of turf toe in football, there have been little data on current players and the shoe wear/playing surfaces currently in use. However, Brophy et al2 evaluated the incidence of turf toe in 44 players on one National Football League team in a 2009 article. In this study, turf toe injury had occurred in 30% of players. Although the cohort was too small to suggest a true reduction in the incidence of this condition from the 45% rate reported by Rodeo et al, this research suggests that turf toe remains a very common entity despite improvements in shoe wear (improved cleat design and stiffer soles) and the advent of newer artificial playing surfaces. Clearly, there exists a research opportunity to determine if newer shoe wear options and playing surfaces (e.g., FieldTurf) affect the incidence of turf toe in American football.
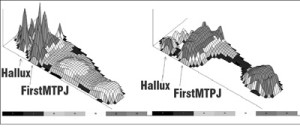
Because turf toe is often considered a “minor” injury not often treated with surgery, the long term sequelae of this injury are not known. However, Clanton noted a 50% incidence of persistent symptoms at the first MTP joint in patients with turf toe who were followed for more than five years after injury.7 In addition, Brophy et al2 found that first MTP dorsiflexion was significantly diminished in NFL players with a history of turf toe compared to those with no history of the same injury. In addition, peak contact pressures under the hallux were significantly increased in players with a history of turf toe (Figure 2). The combination of these two findings suggests a mechanism by which symptoms of turf toe could persist, but further research is needed to determine if contact pressures or limited range of motion actually correlate with the severity or duration of symptoms.
Pathoanatomy, Classification, and Diagnosis
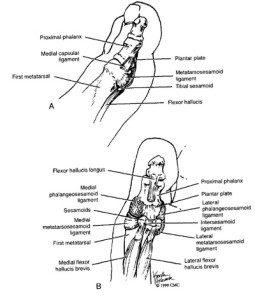
The rounded first metatarsal head articulates with the shallow concave proximal phalanx. This bony articulation offers little overall stability but is supported by strong ligaments, particularly the medial and lateral collateral ligaments, which inhibit most abduction and adduction. The motion of the MTP joint is primarily flexion and extension. Turf toe injuries caused by pure hyperextension often injure the complex plantar structures of the MTP joint. In a 2000 article, Watson et al8 provide a detailed description of the anatomy and pathoanatomy of this injury. The plantar structures of the first MTP joint are a confluence of the strong plantar plate, the collateral ligaments, the sesamoid complex, and the flexor/abductor/adductor hallucis muscles (Figure 3). With forced first MTP joint dorsiflexion, the joint capsule commonly tears off the metatarsal head since it is more firmly attached to the proximal phalanx.4
Clanton and Ford proposed a useful classification of turf toe injury in their 1994 article.7 It is important to note that not all injuries fall within the three grades, but the classification remains useful as it provides a rough estimate of injury severity.
A grade 1 turf toe injury represents a stretch injury or sprain of the plantar capsuloligamentous complex. Typically a patient with a grade 1 sprain may finish the game or practice and report pain in the MTP joint, but may not recall the exact play during which the injury occurred. Diagnosis is usually supported by mild to moderate tenderness upon palpation of the plantar aspect of the MTP joint and pain with passive terminal dorsiflexion of the joint. Weight bearing is usually tolerable and swelling minimal.
A grade 2 turf toe injury reflects a partial tear of the plantar capsuloligamentous complex. These patients present with swelling and pain during weight bearing and often guard against passive dorsiflexion. A grade 3 turf toe injury represents a complete tear with avulsion of the plantar plate from the metatarsal head. These players present with increased swelling and ecchymosis, severe tenderness, and are often unable to bear weight on the forefoot.
Imaging
Plain films including anteroposterior, lateral and oblique views of the foot should be obtained in all but the most minor cases of turf toe. These films can rule out hallux fracture, proximal migration of the sesamoids, a bony capsular avulsion, sesamoid fracture, and diastasis of the sesamoids.9,10 A contralateral foot series is also helpful to evaluate the patient’s normal sesamoid anatomy and sesamoid-to-joint distance.8 We also obtain an MRI in athletes with turf toe who are unable to bear weight comfortably, as it provides valuable diagnostic information about the specific structures injured and can be a valuable prognostic tool for return to play as well.8 Details of the MRI findings on acute turf toe are beyond the scope of this review, but are nicely reviewed in a 2008 paper by Crain et al.11
Treatment
Treatment of turf toe in football is dependent on the grade and severity of the hyperextension injury. The successful nonoperative treatment of turf toe injuries is well documented.8,9,12,13 Athletes with grade 1 injuries often miss little or no playing time. These athletes are treated with nonsteroidal anti-inflammatory drugs (NSAIDs) and rest, ice, compression, and elevation (RICE). Immobilization is rarely necessary. Athletes can often return to play with a combination of “turf toe taping,” shoe wear modification, or application of a more rigid insole. Taping is performed by bringing loops of a 1 to 2 cm wide piece of athletic tape (reinforced with moleskin) from the dorsal surface of the great toe to the plantar surface to prevent dorsiflexion beyond 30º.
Athletes with grade 2 injuries often are more comfortable with a walking boot for a few days followed by progressive mobilization by the athletic trainer. The typical American football player with a grade 2 turf toe injury will miss one to two weeks of competition but may have persistent symptoms during games or practice upon returning to play. Grade 3 injuries documented on MRI will need a period of immobilization and protected weight bearing (with or without a cast in slight MTP plantar flexion, and may require four to six weeks before return to play. In general, the return of painless passive terminal dorsiflexion is an indication to progress an athlete to running followed by cutting and drills.8,9 Hard running should be painless prior to sport specific drills and cutting. Since skill position players (e.g., wide receivers, defensive backs, running backs) may tolerate less in the way of shoe modification and modalities to limit first MTP range of motion, they may take longer for a full return to competition.
Nonoperative treatment of turf toe injuries is usually successful in returning athletes to play, but there is a subset of athletes that will require early surgery. Indications for acute surgery in turf toe hyperextension injuries are not well established but could include loose bodies, MTP joint instability, sesamoid fracture, proximal migration of the sesamoids, or diastasis of sesamoids.8,10 Athletes who fail optimal nonoperative treatment may require late surgery. The surgical management of these players is discussed by Watson et al8 and McCormick et al.14
Conclusion
Turf toe remains a common problem in American football. This injury historically has been a “grab bag” diagnosis including any problem with the first MTP in athletes. However, the literature suggests the diagnosis of turf toe should be defined as injury of the plantar aspect of the first MTP joint when the joint is forcibly hyperextended. Because the literature discussing turf toe injuries is entirely retrospective and largely historical, the current incidence of this condition is unknown. More current prospective epidemiological studies would be beneficial since turf toe represents an injury with great potential for prevention through the optimization of shoe wear and playing surfaces. Turf toe injury does cause a lasting decrease in first MTP motion and increased plantar foot contact pressures in football players.2,4 Despite these sequelae, it is clear that grade 1 and 2 turf toe hyperextension injuries have good outcomes when treated non-operatively. The optimal treatment for grade 3 turf toe injuries with complete capsular avulsion remains unknown. Prospective collection of data on this injury would: 1) be beneficial in determining the incidence of turf toe, 2) aid in developing preventive strategies for this injury, and 3) determine the optimal treatment for the more severe injuries.
Seth C. Gamradt, MD, is an assistant professor of orthopaedic surgery and sports medicine at the University of California Los Angeles. Robert H. Brophy, MD, is an assistant professor of orthopedic surgery at Washington University in St. Louis.
References
1. Bowers KD Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports 1976;8(2):81-83.
2. Brophy RH, Gamradt SC, Ellis SJ, et al. Effect of turf toe on foot contact pressures in professional American football players. Foot Ankle Int 2009;30(5):405-409.
3. Frey C, Andersen GD, Feder KS. Plantarflexion injury to the metatarsophalangeal joint (“sand toe”). Foot Ankle Int 1996;17(9):576-581.
4. Rodeo SA, O’Brien S, Warren RF, et al. Turf-toe: an analysis of metatarsophalangeal joint sprains in professional football players. Am J Sports Med 1990;18(3):280-285.
5. Clanton TO, Butler JE, Eggert A. Injuries to the metatarsophalangeal joints in athletes. Foot Ankle 1986;7(3):162-176.
6. Coker TP, Arnold JA, Weber DL. Traumatic lesions of the metatarsophalangeal joint of the great toe in athletes. Am J Sports Med 1978;6(6):326-334.
7. Clanton TO, Ford JJ. Turf toe injury. Clin Sports Med 1994;13(4):731-741.
8. Watson TS, Anderson RB, Davis WH. Periarticular injuries to the hallux metatarsophalangeal joint in athletes. Foot Ankle Clin 2000;5(3):687-713.
9. Mullen JE, O’Malley MJ. Sprains–residual instability of subtalar, Lisfranc joints, and turf toe. Clin Sports Med 2004;23(1):97-121.
10. Rodeo SA, Warren RF, O’Brien SJ, et al. Diastasis of bipartite sesamoids of the first metatarsophalangeal joint. Foot Ankle 1993;14(8):425-434.
11. Crain JM, Phancao JP, Stidham K. MR imaging of turf toe. Magn Reson Imaging Clin N Am 2008;16(1):93-103.
12. Kubitz ER. Athletic injuries of the first metatarsophalangeal joint. J Am Podiatr Med Assoc 2003;93(4):325-332.
13. Nihal A, Trepman E, Nag D. First ray disorders in athletes. Sports Med Arthrosc 2009;17(3):160-166.
14. McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin 2009;14(2):135-150.
Figure captions:
Figure 1. The most common mechanism of injury in turf-toe is a hyperextension injury to the first metatarsophalangeal joint. The joint capsule tears off of the metatarsal head since the attachment is weaker at this site than at the proximal phalanx. (Reproduced with permission from Rodeo et al AJSM 18:280-285.)
Figure 2. Three-dimensional representation mapping peak pressures in players with (A) and without (B) turf toe. Note that although the peak MTP and hallucal pressures both appear higher in the player with turf toe, a statistically significant difference was found only in the hallux across all subjects. (Reproduced with permission from: Brophy RH, Gamradt SC, Ellis SJ, Barnes RP, Rodeo SA, Warren RF, Hillstrom H. Foot Ankle Int. 2009 May;30(5):405-409.)
Figure 3. The capsular-ligamentous-sesamoid complex of the hallux. A.Medial view. B. Plantar vies. (Reproduced with permission from Bowman MW: Athletic injuries of the great toe metatarsophalangeal joint. In Adelaar RS (ed): Disorders of the Great Toe. Rosemont, IL, American Academy of Orthopaedic Surgeons, 1997, pp 1-22)