 Myofascial or joint-focused stretches can increase passive hip range of motion in young adult men with limited hip flexibility, but this will not necessarily result in more hip motion actually being utilized during functional activity unless old movement patterns can be unlearned.
Myofascial or joint-focused stretches can increase passive hip range of motion in young adult men with limited hip flexibility, but this will not necessarily result in more hip motion actually being utilized during functional activity unless old movement patterns can be unlearned.
By Janice Moreside, PhD
My research on hip flexibility was driven by long-standing anecdotal clinical evidence of a group of young healthy adults with marked limitation of passive hip range of motion (ROM). Typically, the most notable limitations are in hip extension and rotation, possibly because limitations in flexion or abduction and adduction are not as obvious, given that end-range motion is not often required during functional activities.
Although some people with limited hip mobility are somewhat deconditioned and sedentary, the trend is anecdotally more apparent in the athletic population. In Canada, the athletes most frequently presenting with this pattern are those who play ice hockey and football (American style), in which there is an emphasis on a forward flexed posture, including hip flexion. Particularly in hockey, players seldom fully extend their hip joints: the drive for forward propulsion comes from hip abduction and lateral rotation, likely resulting in strengthening and hypertrophy of these muscle groups, subsequent decreased extensibility, and eventual loss of hip extension and internal rotation ROM.
The current literature is unclear regarding “normal” ROM in a young adult population, due to variations in participant position during testing (supine, prone, or sitting), measurement methodology (e.g., goniometer vs inclinometer, active vs passive), and gender. ROM is frequently stated as a group average, plus or minus standard deviation, with no indication of percentile data. Thus, our first step in this line of research was determining “normal” hip ROM, including percentile data, in a group of young healthy adult men; we did not analyze women at this time, since their hip ROM has been shown to differ from men.1-3 Once we determined a normal range for hip ROM, the question arose as to the potential for changing hip ROM in the limited hip mobility cohort. Could we take a group of young men with “tight hips” and bring them into a more normal or even highly flexible range? And, if so, would it make any difference to their functional movement? That is, does an increase in passive ROM result in increased ROM utilized during functional activity?
Quantifying hip ROM
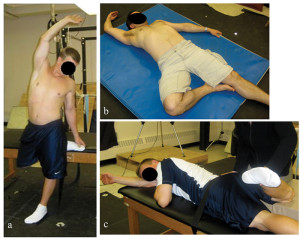
Figure 1: Examples of whole body stretches incorporating myofascial principles aimed at increasing hip external rotation: a) and b) are self-stretches and c) is manual stretching by the researcher. Note that in each case the right arm is elevated and, when possible, the torso is twisted to the left and the hip extended to maximize tension in the entire right anterior aspect of the body. (Reprinted with permission from reference 7.)
Our first step was quantifying hip ROM in healthy young adult men.4 Although this would appear to be a straightforward study, there were a few surprising outcomes. In a group of 77 men, we obtained the following passive hip ROM measures: extension, using the Modified Thomas test5 with the participant supine and a blood pressure cuff under the lumbar spine to monitor lordosis; internal rotation (IR); and external rotation (ER), measuring both rotations in prone and supine positions.
All positional data were captured using a Vicon motion capture system, followed by mathematical calculations of joint angles. We also measured hip extension and prone rotations with a goniometer in a subgroup of 22 participants.
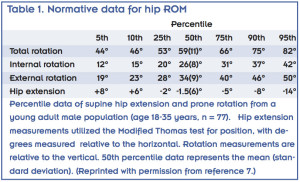
We recorded numerous findings relevant to the practicing clinician. First, we now have normative data for hip ROM, detailing from the 5th to the 95th percentile (Table 1), which is useful information to share with patients when discussing their ROM. There were no significant differences between the goniometer and motion capture measurements for internal rotation, external rotation, and total rotation, and though the goniometer consistently measured approximately 3.9° more extension than the motion capture system, there was still a high correlation. Given this knowledge, the clinician can confidently measure hip rotation and extension with a goniometer, knowing that it correlates well with a more high-tech (and expensive) motion capture system, and thus embark on clinical research projects of their own. One of the surprising outcomes was the poor correlation between total rotation and extension. One participant, for example, was in the 95th percentile for total hip rotation but the 30th percentile for extension, while another had the opposite trend, with hip rotation in the 10th percentile and hip extension in the 95th percentile. Thus, this group of young men did not follow the capsular pattern of restriction that is more commonly seen in the aged or arthritic hip.6 Limitation in one direction does not imply limitation in the other, thus clinicians need to be cautious about such assumptions.
Similarly, there was a weak correlation between supine and prone rotation measurements. While it may not be surprising that significantly more IR exists in a prone position (26 ± 10° vs 11 ± 11° in supine; r2 = .36), and ER is greater in a supine position (38 ± 10° vs 35 ± 9° in prone, r2 = .23), there was also significantly more total hip rotation when participants were lying prone (61 ± 12° vs 49 ± 12° in supine, r2 = .23), suggesting that passive structures limiting hip rotation are tighter in a supine position (with the hip flexed to 90°) than in a prone position. Thus, what may appear to be limited hip mobility when in supine may, in fact, be a function of the test position. To understand available hip rotation accurately, prone measurements are also advisable, as the correlations between supine and prone rotations are not strong.
Hip ROM interventions
 After determining what constituted limited hip mobility, the next step7 was obtaining volunteers whose hip extension and rotation ROM were both lower than the 50th percentile. Of the 250 men screened, only 24 fit these criteria. The participants were randomly assigned to four different six-week intervention groups: group one, hip stretching; group two, hip stretching combined with hip/spine disassociation exercises; group three, core endurance/strengthening (no stretching) combined with hip/spine disassociation exercises; and group four, controls, who were instructed to continue with their current exercise routine. We asked participants to do the exercises at least five times per week.
After determining what constituted limited hip mobility, the next step7 was obtaining volunteers whose hip extension and rotation ROM were both lower than the 50th percentile. Of the 250 men screened, only 24 fit these criteria. The participants were randomly assigned to four different six-week intervention groups: group one, hip stretching; group two, hip stretching combined with hip/spine disassociation exercises; group three, core endurance/strengthening (no stretching) combined with hip/spine disassociation exercises; and group four, controls, who were instructed to continue with their current exercise routine. We asked participants to do the exercises at least five times per week.
Stretches were based on the principle that myofascial connections transmit forces to adjacent musculotendinous structures in series and parallel,8-10 and that a more thorough stretch would occur if aimed not only at the hip joint specifically, but also at the fascial connections overlying the portion of the hip joint under tension. Thus, given that ER is limited by the joint capsule, y-ligament,11 and muscles anterior to the hip joint,5 a stretch to increase right hip ER was performed with the hip in a non-flexed position, the right arm elevated, and the torso twisted/side bent to the left (Figure 1).
These stretches were not designed in accordance with any former precedent, but were anecdotally appreciated by the participants, many of whom embraced them as being “different” from previous stretching protocols with regard to the resulting tension that ensued.
Hip/spine disassociation exercises (groups two and three) focused on maintaining a stable core while moving the hip through various ranges of motion to help participants understand where motion was occurring (at the hip vs the spine). Core exercises (group three) included endurance and strengthening/coordination exercises such as planks, side bridges,12 bent knee fall-outs,13 and a suitcase walk.14 The investigator (a registered physiotherapist) pro- gressed all exercises as appropriate over six weeks.
The two groups that received hip stretching protocols demonstrated large increases in ROM, with extension increasing from approximately the 8th to the 75th percentile, and rotation from the 30th to the 85th percentile.
Thus, not only did hip mobility improve, the average hip ROM was now “excessive”—a finding that may not be necessarily beneficial, which is a point discussed in the concluding section of this paper. Of equal interest is that individuals in group 3, who received no stretching, also showed increased hip ROM on all outcome measures, including significant average improvements of 18% for IR and 10% for total rotation. The control group showed no significant changes in ROM.
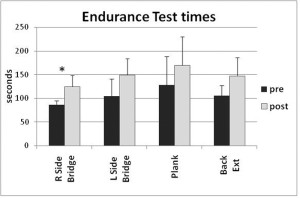
Figure 2. Endurance measured in seconds for the four test positions as labeled (n = 6pergroup). *Significanceatp=.0125
While this research demonstrates that combining myofascial concepts with traditional hip stretches results in large increases in ROM, it is not possible to comment on whether such improvements would have occurred with joint-focused stretches alone.
These results are similar to those found by Winters et al15 in a group of young men (average age 23.6 ± 5 years) with low back pain, who undertook a more joint-focused approach to improve hip extension. However, the stretching protocol in our study provides a treatment alternative that is worth considering in clinical situations. More research needs to be done to fully understand the effect and longevity of myofascial stretches and how best to optimize the protocols.
The finding that hip ROM also improved in group 3 (core stabilization), with no associated hip stretches, is in keeping with the principles of Kibler et al,16 who discuss the importance of core stability for distal mobility. This finding should be a reminder to clinicians that core stabilization exercises may have an important role to play when rehabilitating the lower extremities.
Hip flexibility and mobility
The next step was to determine if improvements in hip flexibility transferred to mobility in functional movement patterns. In a study17 that took place concurrently with the previously described study, functional hip motion was measured before and after the six-week intervention, using a battery of functional movement tasks: a lunge, a “twist and reach” maneuver, active hip extension in standing, and exercising on an elliptical trainer.
The first three tasks were specifically chosen because they are relatively familiar movements that challenge active hip motion and spine control during hip extension and rotation activities. The elliptical task was chosen because exercising on an elliptical trainer is similar to walking, but with increased constraint of foot and hand positions,18 which is likely to improve repeatability within and between subjects.
Despite the aforementioned large improvements in hip extension and rotation, there were no significant increases in hip motion utilized during any of the functional movements tested at the end of six weeks. Participants in groups one and two averaged less hip extension during the lunge, elliptical, and active hip extension than at baseline, though not significantly so. Concurrently, they averaged an increase in the amount of lumbar extension utilized during active hip extension, indicating that, while their focus may have been on positioning the foot further behind the body, they did not differentiate between hip and spine extension.
Similarly, despite core endurance improvements ranging from 23% to 49% (Figure 2), the only indication of constrained spine motion was a significant decrease in lumbar rotation during active hip extension across all groups. It appears participants had more difficulty monitoring pelvic and lumbar flexion/extension than rotation around a vertical axis, possibly because the latter offers greater visual feedback and has an obvious midpoint of zero. However, it is important to build awareness of lumbo-pelvic positioning when rehabilitating the lower limb, as repetitive flexion/extension and/or rotation of the lumbar spine have been linked with lumbar disc degeneration.19-21
Clinical implications
Our findings suggest that hip flexibility can be greatly improved in this young adult male cohort. Clinicians are encouraged to experiment with different myofascial stretches, in addition to those that are more joint-focused; there is no evidence at this time that either stretching technique is superior to the other. To the best of my knowledge, there is no research that specifically addresses capsular/ligamentous versus muscular stretches at the hip joint, and it may be that differing etiologies of limited mobility respond better to one technique or the other.
This work lends credence to the importance of core stabilization, endurance, and awareness when the desired outcome is limb motion. Core or proximal stiffening provides a base for the limb movement,16,22 facilitating increased passive hip ROM.7 However, this increased passive ROM does not automatically transfer to function; in order for new motor patterns to be adopted, old patterns must be overcome.23,24 Movement patterns that utilize newfound joint motion during relevant functional activities must be practiced repeatedly and “grooved” if they are to become incorporated into “normal movement.”
Finally, a word of caution. Not everyone requires increased hip flexibility. Depending on an individual’s athletic needs, musculoskeletal health, and numerous other factors, a little tightness may be a good thing. In a group of young men using the elliptical trainer, gluteus medius activity averaged 45% of maximum voluntary contraction (MVC) in those with excessive hip mobility, compared with 28% MVC demonstrated by those with limited mobility.25 This resulting increase in muscle activity comes at a metabolic cost, and may be partly explained by a diminished ability of the “loose” hips to store and release elastic energy in the passive and musculotendinous structures 26-28 when constrained to a similar stride length and width. Optimal hip flexibility should therefore be determined on a case-by-case basis, depending on perceived activity requirements and hip joint skeletal configuration, as well as current or anticipated musculoskeletal pathologies.
Janice Moreside, PhD, is a registered physiotherapist and an assistant professor in the School of Health and Human Performance at Dalhousie University in Halifax, Nova Scotia, Canada.
Acknowledgements: This work could not have taken place without the mentorship and support of Stuart McGill, PhD, at the Spine Biomechanics Laboratory, University of Waterloo, Canada. Funding assistance was supplied by the Natural Sciences and Engineering Research Council of Canada.
1. Simoneau GG, Hoenig KJ, Lepley JE, Papanek PE. Influence of hip position and gender on active hip internal and external rotation. J Orthop Sports Phys Ther 1998;28(3):158-164.
2. Dolan P, Adams MA. Influence of lumbar and hip mobility on the bending stresses acting on the lumbar spine. Clin Biomech 1993;8(4):185-192.
3. Gombatto SP, Collins DR, Sahrmann SA, et al. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clin Biomech 2006;21(3):263-271.
4. Moreside JM, McGill SM. Quantifying normal 3D hip ROM in healthy young adult males with clinical and laboratory tools: Hip mobility restrictions appear to be plane-specific. Clin Biomech 2011;26(8):824-829.
5. Kendall FP, McCreary EK. Muscles, Testing and Function. 3rd ed. Baltimore: Williams & Wilkens; 1983.
6. Magee DJ. Orthopedic Physical Assessment. Philadelphia, PA: W. B. Saunders Company; 1987.
7. Moreside JM, McGill SM. Hip joint ROM improvements using three different interventions. J Strength Cond Res 2012;26(5):1265-1273.
8. Myers TW. Anatomy trains: Myofascial Meridians for Manual and Movement Therapists. New York: Churchill Livingstone; 2001.
9. Huijing PA, Baan GC. Myofascial force transmission via extramuscular pathways occurs between antagonistic muscles. Cells Tissues Organs 2008;188(4):400-414.
10. Carvalhais VO, Ocarino Jde M, Araujo VL, et al. Myofascial force transmission between the latissimus dorsi and gluteus maximus muscles: an in vivo experiment. J Biomech 2013;46(5):1003-1007.
11. Gray H. Gray’s Anatomy. Philadelphia, PA: Running Press; 1974.
12. McGill SM. Low Back Disorders. Champaign, IL: Human Kinetics; 2002.
13. Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. USA: Elsevier; 2002.
14. McGill SM. Ultimate Back Fitness and Performance. Waterloo, Ontario: Wabano Publishers; 2004.
15. Winters MV, Blake CG, Trost JS, et al. Passive versus active stretching of hip flexor muscles in subjects with limited hip extension: A randomized clinical trial. Phys Ther 2004;84(9):800-807.
16. Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med 2006;36(3):189-198.
17. Moreside JM, McGill SM. Improvements in hip flexibility do not transfer to mobility in functional movement patterns. J Strength Cond Res 2013;27(10):2635-2643.
18. Moreside JM, McGill SM. How do elliptical machines differ from walking: A study of torso motion and muscle activity. Clin Biomech 2012;27(7):738-743.
19. Callaghan JP, McGill SM. Intervertebral disc herniation: studies on a porcine model exposed to highly repetitive flexion/extension motion with compressive force. Clin Biomech 2001;16(1):28-37.
20. Tampier C, Drake JD, Callaghan JP, McGill SM. Progressive disc herniation: an investigation of the mechanism using radiologic, histochemical, and microscopic dissection techniques on a porcine model. Spine 2007;32(25):2869-2874.
21. Marshall LW, McGill SM. The role of axial torque in disc herniation. Clin Biomech 2010;25(1):6-9.
22. Hewett TE, Myer GD. The mechanistic connection between the trunk, hip, knee, and anterior cruciate ligament injury. Exerc Sport Sci Rev 2011;39(4):161-166.
23. Caillou D, Nourrit D, Deschamps T, et al. Overcoming spontaneous patterns of coordination during the acquisition of a complex balancing task. Can J Exp Psychol 2002;56(4):283-293.
24. Delignières D, Nourrit D, Sioud R, et al. Preferred coordination modes in the first steps of the learning of a complex gymnastics skill. Hum Mov Sci 1998;17(2):221-241.
25. Moreside JM. The Effect of Limited Hip Mobility on the Lumbar Spine in a Young Adult Population [dissertation]. Waterloo, Ontario: University of Waterloo; 2010.
26. Sawicki GS, Lewis CL, Ferris DP. It pays to have a spring in your step. Exerc Sport Sci Rev 2009;37(3):130-138.
27. Alexander RM, Bennet-Clark HC. Storage of elastic strain energy in muscle and other tissue. Nature 1977;265(5590):114-117.
28. Kubo K, Kawakami Y, Fukunaga T. Influence of elastic properties of tendon structures on jump performance in humans. J Appl Physiol 1999;87(6):2090-2096.







