By Keith Loria
The development of foot orthotics—both their prescription designs and their manufacturing processes—is continuously evolving as new materials and new manufacturing technologies arise to meet the changing demands of today’s medical and sport performance needs. Just as medical practitioners have pushed the range of foot and lower limb pathologies for which these medical devices can be used, so too have manufacturers pushed the technology to improve the technical aspects of the product as well as the speed of manufacturing.
At a recent lerEXPO virtual event, “Orthotic Treatment Through the Ages” sponsored by ARIZE, authorities in the field of orthotics offered their thoughts on the processes for designing and manufacturing of today’s orthotics.
Prescription Design
First up was Craig Payne, DipPod, MPH, a podiatrist and noted university lecturer from Australia, who focused on the various steps available to get “from the foot to the orthotic” and how those have evolved.
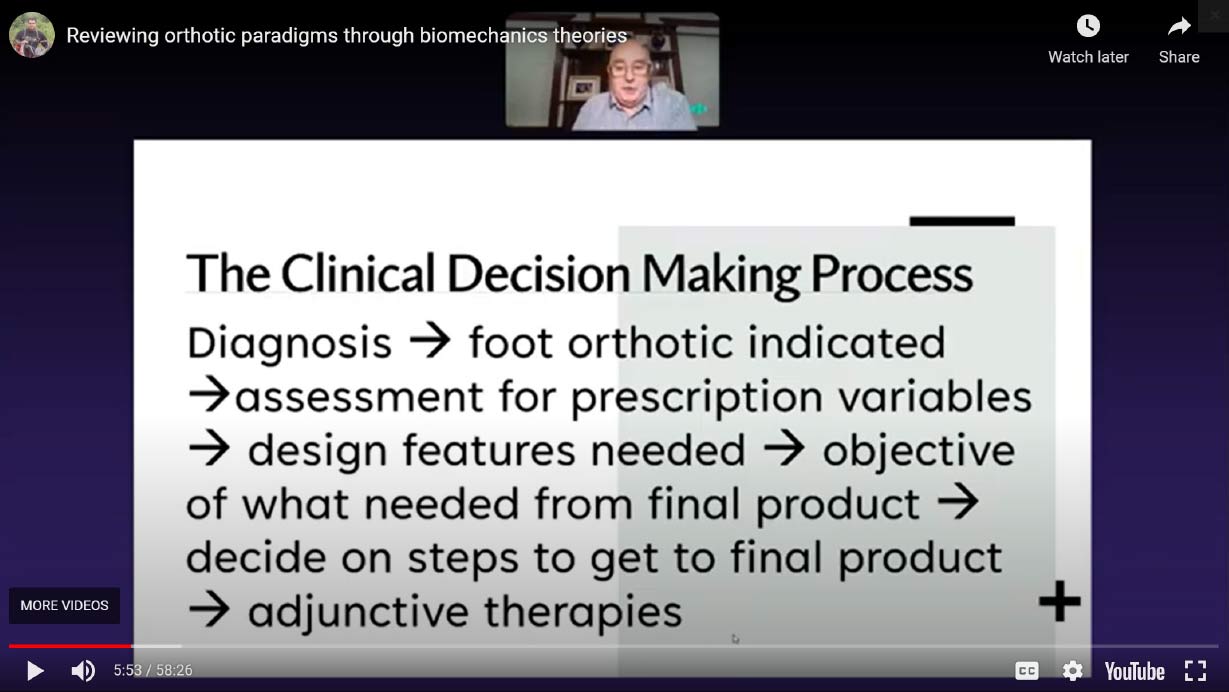
“I look at it as a clinical decision-making process,” he said (Figure 1). “Once you make a diagnosis (eg, posterior tibial tendon dysfunction or plantar fasciitis), somewhere around that diagnosis a foot orthotic is indicated.” To determine the specific needs, assessments are performed, such as gait analysis or postural alignment. These assessments, he explained, are done to look for “prescription variables.” Once those are known, design features of the orthotic are identified “to get the result of what we want.”
“Then we have to decide on the steps to get to the final product, and those are the steps we’ll go through” he said, adding, “of course, we’ll do the necessary adjunctive therapies (eg, stretching or muscle rehab)…but I’m going to focus on deciding on the steps for how we get to the final [foot orthotic] product.”
“We start with making a negative model,” he said (Figure 2). “in the past, we called it a cast.”
There are countless challenges with the negative models including: weightbearing versus non-weightbearing versus partial weightbearing; foot positioning (STJ neutral, MASS, facilitate windlass, etc.); prone or supine; forefoot varus or supinatus; capture rear of calcaneus; hands on or off the foot; and alignment/posture vs kinetics/loads. While acknowledging that the debate continues to rage, Payne was clear that for the last item, at least, he believes kinetics/load are most important.
 He then described the many methods available to obtain the negative model, noting the many “new” technologies that have come and gone:
He then described the many methods available to obtain the negative model, noting the many “new” technologies that have come and gone:
- eyeballing (“this is really just looking at the foot”)
- plaster cast (depends on the skill of the technician)
- STS sock (“similar to the plaster cast but less greasy”)
- foam box
- optical scanners (“many of today’s models connect with iPads or iPhones, but there remain issues with holding the foot in proper position)
- photogrammetry (“involves taking several 2D photographs of the foot and providing measurements such that an algorithm can translate into a 3D image of the foot from which you can create a model… The evidence is pretty good”)
- dilatancy-based systems (dilatancy is defined as the volume change observed in granular materials when they are subjected to shear deformations)
- weight-bearing systems (“these allow you to change the alignment of the foot in real time”)
- pin matrix systems (“in these, non-sharp pins come up from below to capture the shape of the arch and the foot”)
- extrapolation based systems (which are not as common today, “do not collect any volumetric data, they collect pressure data, and they rely on an algorithm to extrapolate that 2D pressure data and somehow create a foot orthotic.”)
Payne cited data from a 20-year-old study showing the cost benefit analysis of using scanning (total costs $3.30–10.00) versus casting ($27.94–$49.60). “Optical scanning was a total no-brainer,” he said.
“Which is the best way [to create a negative model]? It comes down to personal preferences and logical fallacies, there are lots of opinions,” Payne said. “There’s no evidence that any one way is better than another.”
The key question he asks is this: “Can you get the segments of the foot in the position that you need?”
The next step involves the decision to use a prefabricated shell or a library device and produce a digital negative model for use by inhouse designers or to be sent out to lab.
“If we have a physical model from plaster, we can then manufacture ourselves, or we can ship it to the lab, or we could scan it and send it to the lab and they will scan it, and then have a digital negative model,” he said.
One of those options is a 3D-printed physical positive model.
“The thing about 3D printing is that once the design process is finished, the lab can print it and send it back to you as a finished product,” Payne said. “Some labs are actually outsourcing the 3D printing to facilities that have multiple machines.”
He concluded by noting that at the end of day, it doesn’t matter what system one uses, or what method, the shape of the final product should be the same if the prescription was followed by the lab.
“Use the method that allows you to manipulate the thickness of the foot into the position that you need, so that you can deliver the design features that are needed to get the outcomes that you want,” Payne said.
3D: Manufacturing the Future
The second session started with commentary by Bruce Williams, DPM, a Chicago-area podiatrist and consultant with Arize Orthotics, who explained how 3D printing could be best applied to orthotics manufacture, describing how 3D printing technology works, the materials available, and the new design possibilities enabled by additive manufacturing.
“3D printers are here, and have been for a while,” Williams said, noting the COVID-19 pandemic was one of the best things to happen to the 3D printer industry, because more people explored working with them due to manufacturing and shipping issues.
The biggest pushback he’s seen with the use of 3D printers for orthotics comes from those who were using materials that weren’t polypropylene or polypropylene-like, and so they would come out hard and didn’t have a lot of flexibility. Or, if they did have flexibility, they were brittle.
Williams noted that labs are getting to the point where the materials they use are no longer a problem, with a higher use of polypropylene or PA-12 (also called Nylon-12) or something similar that could mimic polypropylene.
“At HP, we use PA-12, and overall, the dimension, the dynamic stiffness, energy recovery, everything is great,” he said. “It’s really difficult to break the thing from a traditional device mounted extension.”
Williams also sees the potential for orthotic devices to be better because of the advanced design potential.
When printing as prescribed, 3D printing allows for prescription modifications to be programmed as needed, at minimal to no additional cost for modification of 3D printed shells that are then is ready to dispense with the addition of a top cover.
“In reality, as we go into the future, the keys are understanding stiffness, thickness, texture, and structure,” he said. “The goals are obviously to have a lighter device, and a thinner device so patients have more room in their shoes, and if we can improve the fit, that’s always a great goal.”
When Williams concluded, Melanie Shelton, Arize product manager at HP with a near 20-year history in orthotics manufacturing, talked further about the 3D capabilities and how to take the concepts and turn them into a solution.
She explained that HP’s approach with the Arize solution was to offer enough standardization that it would be very easy for clinicians to adopt into a clinic but also provide enough innovation and value that it would be significantly better than some of the other solutions that are out there.
“Design consistency and repeatability, that is 100 percent something that we can provide to you,” Shelton said. “That’s something that a 3D printing end-to-end solution can absolutely do for you in ways that cannot be done with these legacy manual processes that you all have experienced.”
Currently, the timeframe to 3D manufacture an orthotic is under 2 weeks and the goal is to continue to get that turnaround time faster and faster.
“Patient outcomes are really important to us and we want happy patients,” Shelton said.
The way it works is a 3D preview of the orthotic design is created so while someone is working with the software and prescribing the orthotic, the design engine is already designing the orthotic at one’s desktop. It takes less than 5 minutes.
“We are able to control thicknesses—thickness on certain modifications and also even able to control thicknesses of the shell itself,” Shelton said. “We’re lucky that in 3D printing, we’re not limited to one-millimeter sheet-stock increments like in legacy processes.”
That means, there can be an orthotic where the arch is a little bit thicker, but under the heel it’s a little bit narrow or shallow, and it also allows for a much lighter weight and a much lower profile orthotic.
Consistency and repeatability of the end-to-end solution were key to building the Arize solution, as was attention to clinician workflow. The goal, Shelton said, “was to ensure that the data is carried all the way through so the orthotic is repeatable and consistent, which is what patients and clinicians want.”
To hear the talks in their entirety, visit lerEXPO.com and go to Events in the top tool bar and search for Orthotic Treatment Through the Ages. While there, scroll through lerEXPO’s other events, all are available for free.