By Danielle Torp, MS, ATC; Luke Donovan, PhD, ATC; Abbey Thomas, PhD, ATC
By Danielle Torp, MS, ATC; Luke Donovan, PhD, ATC; Abbey Thomas, PhD, ATC
Center of pressure is a critical biomechanical measure of human postural control and gait, particularly in chronic ankle instability. Evidence from biofeedback studies reveals COP may be modified to improve gait and functional movement.
Center of pressure (COP), and its response to activity within the sensorimotor system, is an oft-reported biomechanical measure of balance and gait. COP represents the location on the support surface where the pressure from the soles of the feet would be applied if that pressure were concentrated in a single spot.1 COP shifts in response to perturbations in balance and activity within the neuromuscular control system making it an important indicator of sensorimotor impairments.
Impaired COP, specifically relating to its trajectory and velocity of excursion, are frequently studied and reported in patients with chronic ankle instability (CAI) among other neuromusculoskeletal conditions. CAI is a condition estimated to affect upwards of 75% of individuals with a history of lateral ankle sprain (LAS).2 CAI is characterized by recurrent episodes of giving way continuing at least 1 year after the initial LAS.3 Patients with CAI experience dorsiflexion range of motion, ankle strength, balance and neuromuscular control impairments as well as aberrant gait biomechanics. Unfortunately, these symptoms perpetuate a continuum of dysfunction that results in repetitive ankle sprains.
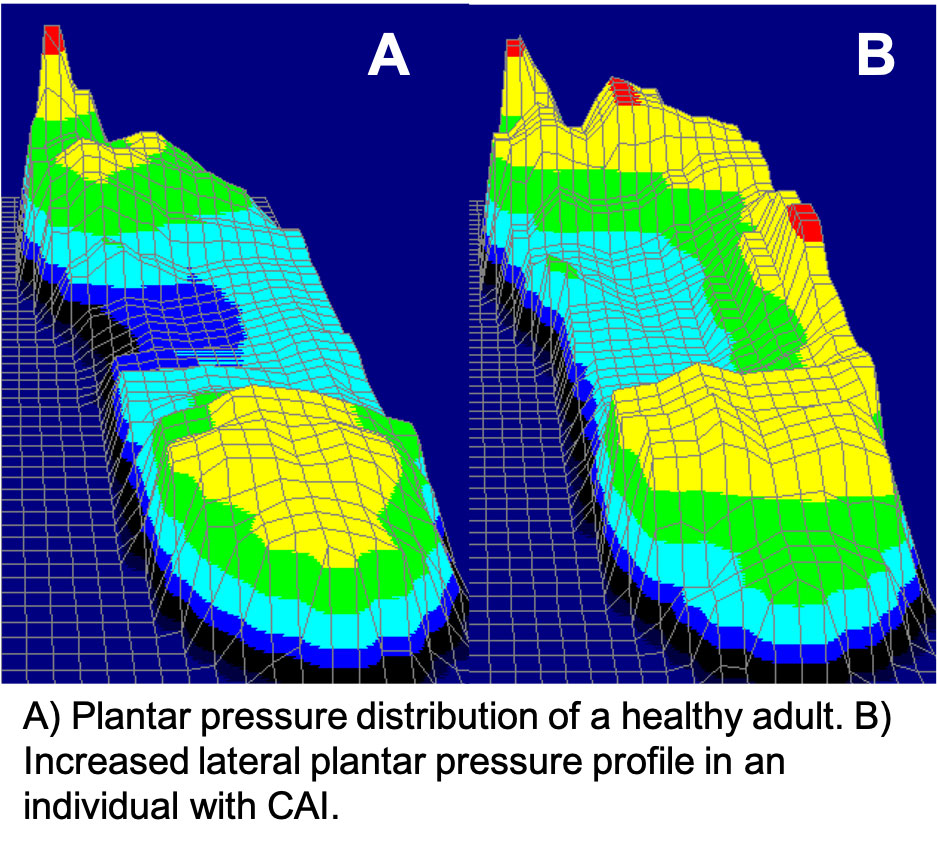
A commonly reported COP deviation in patients with CAI is an increased anterolateral COP during single-limb static balance.4 This aberrant biomechanical profile has also been demonstrated during walking5 and jogging.6 A laterally shifted COP places the foot and ankle in a position where it may be readily inverted, which is problematic considering that excessive ankle inversion is a risk factor for the recurrent injuries sustained by individuals with CAI. This foot position is depicted in Figure 1 representing plantar pressure during walking from which COP is derived. Further complicating the problem of a laterally deviated COP is the impaired neuromuscular activation of the ankle evertor muscles in patients with CAI, hindering their ability to protect against ankle inversion. Fortunately, COP trajectory may be modifiable, representing an avenue through which clinicians can break the continuum of dysfunction associated with CAI.
Current Options for Shifting Plantar Pressure
Current research supports gait training and use of biofeedback devices as a means of changing plantar pressure in patients with CAI.
Gait Training: Feger and Hertel7 developed a gait training device to encourage a medial shift in plantar pressure during treadmill walking. The device consists of two tracks that run parallel to the treadmill belt. The tracks are centrally positioned between the individual’s legs at a height within the distal 1/3 of the individual’s shank. Elastic bands secured to the device’s tracks are wrapped around the individual’s lower leg. The elastic bands applied a medially directed force to the distal shank throughout the gait cycle. A single, 30s walking trial with this gait training device decreased lateral plantar pressure and shifted the COP gait line medially during stance. Notably, this device concurrently increased peroneus longus muscle activity, which may have allowed for greater ankle eversion and the reduction in lateral plantar pressure.
Gait Training with Auditory Biofeedback: Auditory biofeedback can be provided by a device placed in the individual’s shoe. The device can then be set to provide an audible cue when too much pressure is applied to a sensor. Donovan et al8 first tested this concept using a custom-made auditory biofeedback device during a single, 30s walking trial while participants tried to walk in a manner that did not cause the device to make noise. Participants successfully decreased lateral plantar pressure while concurrently increasing peroneus longus muscle activity.
Gait Training with Visual Biofeedback: Our laboratory group has recently developed a visual biofeedback device that can decrease lateral plantar pressure during treadmill walking.9 We secured a cross-line laser pointer to the dorsal surface of the foot and had participants walk on a treadmill facing a wall so they could see the trajectory of the laser pointer on the wall as they walked. Using this setup, laser orientation corresponds to plantar pressure location, such that if a participant rotated the laser laterally that would equate to greater plantar pressure under the lateral column of the foot.10 We applied a piece of tape vertically to the wall and instructed our participants to walk so the vertical laser line was aligned with the tape. They were further instructed not to let the laser deviate left, right, or rotate. Using these instructions for a single, 30s bout of walking, participants successfully decreased lateral plantar pressure and shifted the COP gait line medially.9
Functional Tasks with Biofeedback: Expanding on the auditory and visual biofeedback studies during walking, we recently examined the ability of these devices to change plantar pressure during functional task performance.11 Participants randomly completed single-leg static balance, step-downs, lateral hops, and forward lunges without feedback and with each of the aforementioned auditory or visual biofeedback devices. The auditory biofeedback produced the following changes in plantar pressure: 1) yielded a posteromedial shift in COP during eyes open and eyes closed balance; 2) increased lateral plantar pressure during step-down, suggestive of a closed-pack position at initial contact to increase stability; and 3) decreased lateral forefoot pressure-time integral during forward lunges.11 Visual biofeedback also changed plantar pressure. Specifically, visual biofeedback produced a posteromedial shift in COP during eyes open balance and increased lateral peak pressure and pressure time integral during lateral hopping.11 The increased lateral pressure during hopping resulted in the previously described closed-pack position believed to increase stability and limit LAS risk.
Collectively, these studies confirm that plantar pressure is modifiable in patients with CAI during a variety of daily and functional tasks. Unfortunately, there are a number of challenges that face clinicians in attempting to change plantar pressure to reduce recurrent LAS in those with CAI.

Figure 2. COP gait line data. The solid green line represents average COP gait line trajectory from initial contact through toe-off of the stance phase. The shaded green region represents deviation from average. Clinicians could expect individuals to respond to an intervention by walking with a COP gait line somewhere in the shaded region, but not necessarily along the solid line.
Challenges of Changing Plantar Pressure
Although the previously mentioned studies appear promising and report similar patterns in altering plantar pressure, their prolonged effects in patients with CAI or use in other patient populations have yet to be explored. Clinicians seeking to adjust foot position, plantar pressure, or biomechanics have often relied on the use of orthotics.12 Conceptually, orthotics can be used to place the foot in a subtalar neutral position thus “placing the ligaments in a more optimal position to allow joint mechanoreceptors to detect abnormal motion.”13 Orthotics have also been ascribed with the ability to reduce range of motion at the ankle, improve tactile sensation, and reduce muscular strain around the ankle making them an ideal candidate to improve biomechanical function.14 Moreover, patient compliance is easily achieved with this intervention compared to other more hands-on approaches. However, there is a lack of consensus about their efficacy in changing plantar pressure or COP.
A common biomechanical risk factor for many lower extremity injuries is excessive pronation or supination during initial phases of stance. This excessive motion will alter the COP trajectory throughout the stance phase and potentially alter proximal joint biomechanics. In an attempt to neutralize the foot and centralize the COP trajectory, clinicians will add a medial or lateral wedge to the orthotic depending on the accessory motion. For example, a supinated or inverted foot at initial contact will produce a laterally deviated COP and increased lateral plantar pressures during stance;15 thereby, a lateral wedge would be inserted to force a neutral foot during the loading phase thus medially shifting COP and reducing lateral plantar pressure. However, research shows an individual’s response while wearing orthotics is variable and inconsistent.16 Some researchers found adding a lateral wedge can shift COP medially and increase medial plantar pressures,17 while other studies reported a lateral wedge had the opposite effect and increased lateral plantar pressure and laterally shifted COP.18
Although the link between orthotics and shifting COP does not appear to be linear, it is important to understand a majority of the aforementioned research focuses on either a healthy population, individuals with diabetes mellitus, or those with flat feet. A smaller portion of this research has focused on patients with overuse injuries, suggesting orthotics may improve patient-reported symptoms.12 The short-term improvements in subjective symptoms reported by patients using orthotics occurs without any significant changes in dysfunctional biomechanics and only in a slight majority of patients. The remaining patients (~40%) complained of new or worsening symptoms from orthotics use. Ultimately, the challenges with using orthotics as a means to shift plantar pressure and COP are the inconsistent findings, lack of understanding which patients will respond positively, and the specific use in patients with ankle sprains.
Limitations of Current Evidence
As previously mentioned, a major limitation to this current body of evidence is the investigation into an injured, athletic population. The inconsistent observations made were in healthy adults and it is unknown how COP of pathological populations would respond to the use of orthotics.
Another major limitation is our current methods for defining, examining, and extracting the COP during gait. Some research has condensed COP to a few discrete data points creating a ‘gait line,’ while others reduce the average COP into a ‘trajectory.’ Both of these methods require the extraction of data along the x- and y-axes of motion. Rarely do researchers examine the real-time, fluctuating journey of the COP during stance. While there is evidence to suggest COP is capable of changing when targeted with gait training and orthotics, there is a lack of patterned effect and predictable response (Figure 2). Perhaps the deductive analysis of measuring COP is hindering researcher’s understanding of the true path and changes occurring during interventions.
Future Directions
Although there is evidence that highlights the connection between COP and neuromechanical conditions such as CAI, more research is warranted prior to establishing best-practice guidelines for evaluating and altering COP. First, the underlying mechanism(s) of COP impairments remains unclear. Elucidating the cause of altered COP will enhance the ability to develop intervention techniques that target the specific mechanism rather than the outcome. Next, the onset of impaired COP is often surmised to be a consequence of the original injury rather than a predisposition to the index injury. In reality, there are limited prospective studies with COP as a primary outcome to truly delineate whether a shift in COP is a risk factor or consequence of injury. Finally, centralizing COP position through biofeedback-based interventions does improve perceived function in patients with CAI; however, these studies did not measure re-injury rates and the follow-up periods were relatively short. As such, going forward, researchers should focus on identifying the mechanisms and onset of altered COP through large prospective cohort studies as well as determining the long-term effects of change COP on injury rates through randomized controlled trials.
Conclusion
The deviations in plantar pressure and COP exhibited by patients with CAI likely play a role in their episodes of giving way and recurring ankle sprains, thus perpetuating the cycle of dysfunction. The disturbance of sensorimotor function in these patients and individuals with other lower extremity joint injuries poses a problem for clinicians working to improve biomechanical function after injury. Ultimately, biofeedback interventions during gait to target the aberrant COP and plantar pressure patterns are promising and warrant inclusion in standard of care rehabilitation for patients with CAI.
Danielle Torp, MS, ATC, is a doctoral candidate in the Department of Kinesiology at the University of North Carolina at Charlotte, Charlotte, North Carolina. Torp’s research interests focus on clinically applicable interventions targeting biomechanical factors influencing long-term joint health and quality of life in patients with lower extremity injuries.
Luke Donovan, PhD, ATC, is an assistant professor in the Department of Kinesiology at University of North Carolina at Charlotte, Charlotte, North Carolina. Donovan’s research efforts work towards improving function and quality of life over the long term in patients with lower extremity joint injury through novel and clinically accessible rehabilitation paradigms.
Abbey Thomas, PhD, ATC, is an assistant professor in the Department of Kinesiology at University of North Carolina at Charlotte, Charlotte, North Carolina. Thomas focuses her research on understanding and treating the neuromuscular and biomechanical consequences of lower extremity joint injuries.
- Winter DA. Biomechanics of Motor Control and Human Movement. 2nd ed. New York: Wiley; 1990.
- Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14; discussion e14.
- Gribble PA, Delahunt E, Bleakley CM, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Athl Train. 2014;49(1):121-127.
- Pope M, Chinn L, Mullineaux D, McKeon PO, Drewes L, Hertel J. Spatial postural control alterations with chronic ankle instability. Gait Posture. 2011;34(2):154-158.
- Koldenhoven RM, Feger MA, Fraser JJ, Saliba S, Hertel J. Surface electromyography and plantar pressure during walking in young adults with chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1060-1070.
- Schmidt H, Sauer LD, Lee SY, Saliba S, Hertel J. Increased in-shoe lateral plantar pressures with chronic ankle instability. Foot Ankle Int. 2011;32(11):1075-1080.
- Feger MA, Hertel J. Surface electromyography and plantar pressure changes with novel gait training device in participants with chronic ankle instability. Clin Biomech (Bristol, Avon). 2016;37:117-124.
- Donovan L, Feger MA, Hart JM, Saliba S, Park J, Hertel J. Effects of an auditory biofeedback device on plantar pressure in patients with chronic ankle instability. Gait Posture. 2016;44:29-36.
- Torp DM, Thomas AC, Donovan L. External feedback during walking improves measures of plantar pressure in individuals with chronic ankle instability. Gait Posture. 2019;67:236-241.
- Donovan L, Torp DM, Thomas-Fenwick AC. Using a Crossline Laser to Predict Peak Plantar Pressure During Walking. J Athl Train. 2020;55(7):739-743.
- Torp DM, Thomas AC, Hubbard-Turner T, Donovan L. Biomechanical Response to External Biofeedback During Functional Tasks in Individuals with Chronic Ankle Instability. J Athl Train. 2020.
- Razeghi M, Batt ME. Biomechanical analysis of the effect of orthotic shoe inserts: a review of the literature. Sports Med. 2000;29(6):425-438.
- Guskiewicz KM, Perrin DH. Effect of orthotics on postural sway following inversion ankle sprain. J Orthop Sports Phys Ther. 1996;23(5):326-331.
- Richie DH, Jr. Effects of foot orthoses on patients with chronic ankle instability. J Am Podiatr Med Assoc. 2007;97(1):19-30.
- Wong L, Hunt A, Burns J, Crosbie J. Effect of foot morphology on center-of-pressure excursion during barefoot walking. J Am Podiatr Med Assoc. 2008;98(2):112-117.
- Aboutorabi A, Arazpour M, Hutchins SW, Curran S, Maleki M. The efficacy of foot orthoses on alteration to center of pressure displacement in subjects with flat and normal feet: a literature review. Disabil Rehabil Assist Technol. 2015;10(6):439-444.
- Nester CJ, van der Linden ML, Bowker P. Effect of foot orthoses on the kinematics and kinetics of normal walking gait. Gait Posture. 2003;17(2):180-187.
- Van Gheluwe B, Dananberg HJ. Changes in plantar foot pressure with in-shoe varus or valgus wedging. J Am Podiatr Med Assoc. 2004;94(1):1-11.