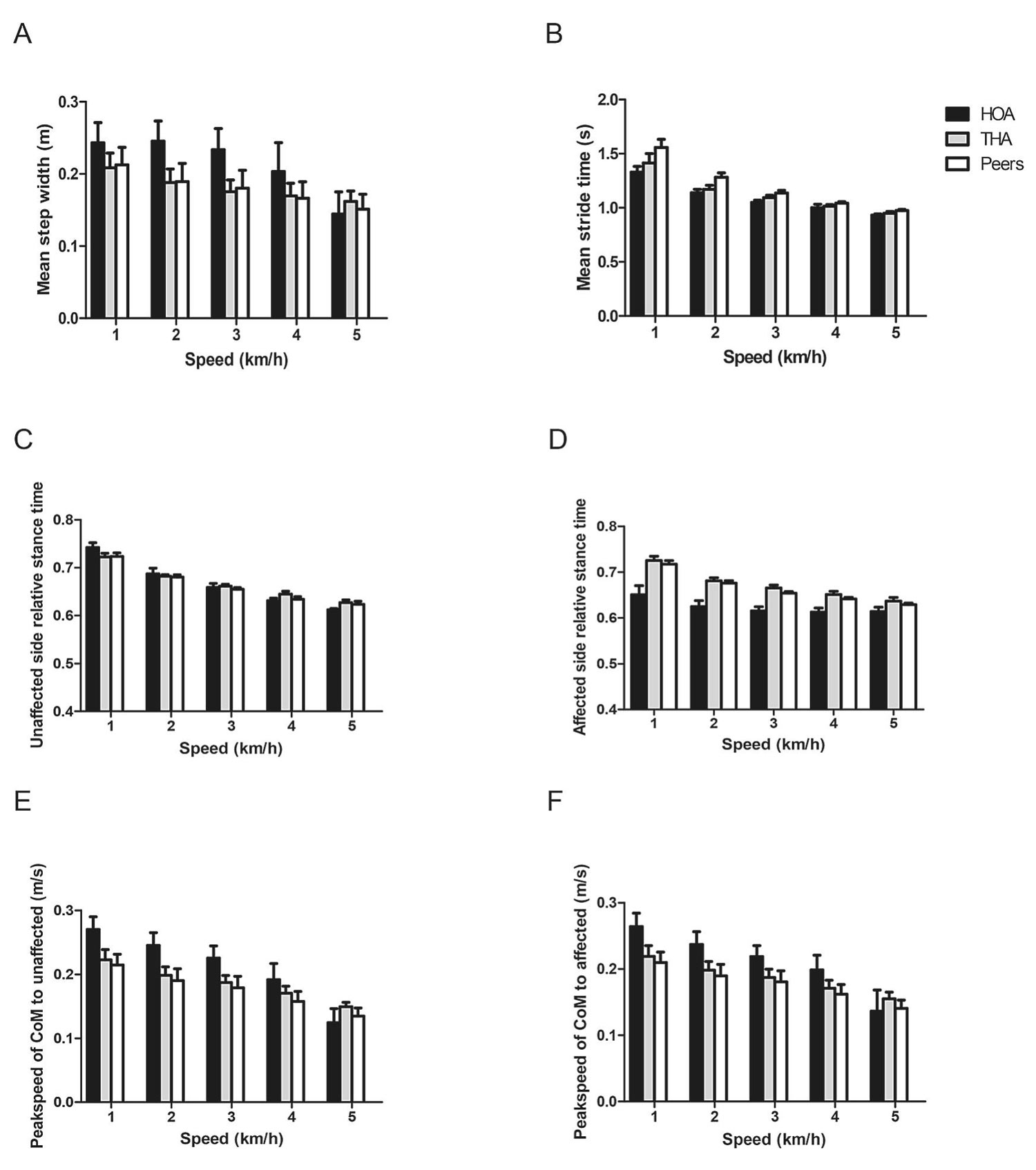
Figure 1. A) Mean step width; (B) Mean stride time; (C) Unaffected side relative stance time; (D) Affected side relative stance time. (E) Peak speed of Center of Mass (CoM) to unaffected side; (F) Peak speed of CoM to affected side. Error bars represent standard errors. Note that the number of subjects was different for the different speeds in both HOA (12, 11, 11, 6, 2, respectively) and THA (12, 12, 12, 9, 8).
Total hip arthroplasty (THA) is the common treatment for end-stage hip osteoarthritis (OA), improving health-related physical function, pain, and quality of life. Still, physical function may not reach the level of healthy controls, and patients report post-operative pain even years after THA.
Falling, per se, is known to have a negative impact on quality of life in the elderly, and fall risk after THA is a serious clinical problem. In the year after THA, around 30%–35% of cases fell at least once. In the first 90 days after THA, 1.6% of patients had a fall incident that was so serious that they had to be hospitalized.
In people with moderate hip OA, gait kinematics was reported to be correlated with number of falls in the preceding year. After THA, patients generally improve but still fall. The present study explores recovery and correlations with number of falls in the year after THA.
This study assessed 12 patients 1 year after THA: 12 patients with moderate hip OA with at least 1 fall in the preceding year, and 12 healthy peers. Maximum hip abduction strength, Fall Efficacy Scale – International, Harris Hip Score, pain, and number of falls in the preceding year were assessed. Participants walked on a treadmill with increasing speeds, and gait kinematics were registered optoelectronically. Group differences were assessed as were correlations of all variables with number of falls.
After arthroplasty, patients tended to score better on variables measured, often non-significantly, compared to patients with moderate OA, but worse than healthy peers (Figure 1). Maximum hip abduction strength together with fall efficacy had a strong regression on the number of falls in the preceding year (R2 = 92%). Gait kinematics did not correlate with number of falls, and also fall efficacy was not related to gait kinematics.
Interpretation: One year after hip arthroplasty, muscle strength sufficiently recovered for normal walking, but not to avoid falling in risky situations—the patients lacked the strength to recover balance. Rehabilitation should focus on muscle strength, particularly the abductors. The lack of correlation between the Fall Efficacy International and gait kinematics suggests that it reflected the experience of having fallen rather than fear.
Source: Lin B, Wu W, Weijer RHA, et al. Strong relationship of muscle force and fall efficacy, but not of gait kinematics, with number of falls in the year after Total Hip Arthroplasty for osteoarthritis: An exploratory study. Clin Biomechanics. 2022;92:105551. Use is per Creative Commons CC BY.