 Total knee arthroplasty significantly improves functional outcomes in obese patients, but is also riskier than in normal-weight patients. As the number of obese patients with knee osteoarthritis continues to rise, clinicians are being challenged to find a balance between the risks and the benefits.
Total knee arthroplasty significantly improves functional outcomes in obese patients, but is also riskier than in normal-weight patients. As the number of obese patients with knee osteoarthritis continues to rise, clinicians are being challenged to find a balance between the risks and the benefits.
By Susan M. Odum, PhD, and Bryan D. Springer, MD
Obesity has reached epidemic proportions, with more than one-half billion obese people living around the world.1 The World Health Organization (WHO) defines overweight as having a body mass index (BMI) between 25 and 29 and obesity as having a BMI of 30 or higher.1 The WHO further classifies obesity as Class 1 (BMI 30-34.9), Class II (BMI 35-39.9), and Class III (BMI > 40).1 It is also common to subcategorize individuals with BMIs from 40 to 49.9 as morbidly obese and those with BMIs of 50 or higher as super obese.2 BMI is the ratio of one’s body weight in kilograms divided by the square of the height in meters (kg/m2).1 This index provides a simple population-level measure of obesity that can be calculated without using special equipment and applied across all demographic groups.1 However, BMI as a measure is limited because it does not consider the composition of body weight (muscle vs adipose tissue) or the distribution of adipose tissue.3
From 1999 to 2008, there was an alarming increase in the proportion of overweight and obese individuals in the US.4 By 2008, the age-adjusted obesity prevalence was 34% and the combined obesity and overweight prevalence reached 68%.4 According to data from the Centers for Disease Control and Prevention’s National Health and Nutrition Examination Survey (NHANES), the rate of obesity in the US appears to have plateaued. The overall prevalence of obesity in the US has remained consistent at 35% to 36% from 2009 to 2012.4-6 The 2009-2010 NHANES data revealed that adults aged 60 years and older were more likely to be obese than younger adults.4,5 We have seen a shift in the age groups, and the prevalence of obesity is now highest among middle-aged adults. Between 2009 and 2010, 39.7% of people aged 60 years or older were obese, compared to 35.4% of people in that age group from 2011 to 2012.4-6 The obesity prevalence for adults aged 40 to 59 years, on the other hand, was 36.6% from 2009 to 2010, compared to 39.5% from 2011 to 2012.4-6
The increase in obesity rates among adults aged 40 to 59 years is noteworthy as it signals a continued increase in the rate of total joint replacement among obese individuals. The average age of total knee arthroplasty (TKA) recipients is decreasing,7 while the proportion of obese TKA patients is increasing.8,9 Fehring et al reported that the prevalence of obesity among total joint replacement patients nearly doubled from 1990 to 2005.9 In 1990, the obesity prevalence in their institution was 30%, compared to 52% in 2005. To put this in perspective, the prevalence of obesity in the US was 34% in 2005.10 Recently, Odum et al analyzed a cohort of more than 750,000 knee replacements performed between 2002 and 2009.8 The authors reported the rate of obesity among TKA patients increased from 6% in 2002 to 20% in 2009.8 After controlling for a number of factors, TKA patients younger than 64 years are four times more likely than older patients to be obese.8 Additionally, Odum et al found that TKA patients who had more than three comorbid medical conditions had a four-fold increased risk of obesity.8
Obesity and osteoarthritis
Evidence shows that increased body weight and obesity are associated with osteoarthritis (OA) of the knee and, ultimately, the need for TKA. In 1988, Felson and Anderson first reported obesity as an independent risk factor for the development of OA.11 In this seminal analysis of the Framingham Study population, the authors reported that, after controlling for age, men in the highest relative, or height-adjusted, body-weight quintile had 1.5 times the risk of developing OA while women in the highest relative body-weight quintile were twice as likely to develop knee OA as individuals with lower relative body weight.
Coggon et al conducted a matched case-control study and found that individuals with a BMI of 36 or higher had a nearly 14 times higher risk of developing knee OA than individuals with a BMI between 24 and 24.9.12 Moreover, the authors concluded that if all people with a BMI of 30 or higher reduced their BMI to within the recommended normal range (18.5 to 24.9) 24% of TKA procedures for OA might be avoided.12 On average, knee OA patients with a BMI of 35 or higher may need TKA surgery seven years earlier than those with BMI levels of less than 25.13 Although TKA implants are designed to last for upwards of 20 years, those who have surgery at younger ages, independent of other risk factors, are more susceptible to additional revision surgery.
Although the link between obesity and knee OA is apparent, the cellular mechanisms by which obesity may contribute to the development of knee OA are not entirely understood. It is beyond the scope of this article to provide a detailed explanation of the cellular process. However, it is important to appreciate the scientific framework for the relationship between obesity and OA. Generally, obesity impacts the biomechanical processes that lead to the degradation of the articular cartilage of the knee and, ultimately, to knee OA.14 The additional body weight associated with high BMI levels produces considerably higher forces on the articular cartilage of weight-bearing joints, such as the knee.14,15 The increased pressure on the joint due to excessive body weight leads to the activation of mechanoreceptors in the knee joint and the subsequent release of metalloproteinases and prostaglandins, which ultimately degrade the articular cartilage.15 Additionally, there are metabolic processes associated with OA.15 Adipose tissue releases cytokines and adipokines, both of which increase inflammation and damage of the articular cartilage.15
Obesity and TKA outcomes
Once the damage to the articular cartilage progresses to the level of bone-to-bone contact, total knee arthroplasty is the definitive treatment to relieve pain and restore functional loss caused by severe progressive OA. Prior published literature reviews have compared functional outcomes between obese and nonobese TKA patients and have reported conflicting findings.3,14,16 A number of studies report no difference in functional outcome between obese and nonobese TKA patients.3,14,16 Other studies report that the functional outcome for nonobese TKA patients is significantly better than for obese TKA patients.3,14,16 There is agreement in the literature that the functional outcome following TKA in morbidly obese patients is significantly worse than in patients who are not obese.3,14,16 However, even if some studies suggest functional outcomes following TKA may be inferior in obese patients compared with nonobese patients, all studies reviewed reported that patients experienced functional improvements compared with baseline levels, regardless of obesity status.3,14,16,17
Patients with BMIs greater than 40 have less functional improvement than patients with lower BMIs, and their rate of improvement is slower.3,14,16 Obese patients undergoing TKA also have an increased risk of medical perioperative complications, such as poor wound healing, infection, respiratory complications, and venous thromboembolism. However, the well-documented increased risk of complications must be evaluated in a medical context; obesity is associated with other comorbid medical conditions that also independently increase the risk of complications.3,14,16 Figure 1 illustrates a wound healing complication in an obese total knee replacement patient.
Technical difficulties
TKA surgery is technically more difficult in patients who have an excessive BMI than in those with lower BMIs.18,19 Järvenpää et al found a significantly higher number of technical errors in a group of obese TKA patients than in nonobese patients.19 The authors noted 17 technical errors in 52 obese patients compared with five errors in 48 nonobese patients.19 Nunez et al measured the level of intraoperative difficulty reported by the surgeon performing TKA as the number of problems that occurred during the TKA surgery.18 The authors found a significantly higher surgeon-reported degree of difficulty associated with morbidly obese patients compared with patients who had BMIs less than 35.18
This degree of difficulty is related to an increased circumference of the leg complicating the surgical exposure of the femur and tibia. The additional layers of adipose tissue make visualization of the structures of knee joint difficult. This limited visualization of the surgical field can lead to technical errors related to inaccurate bone cuts, damage to soft tissue structures, and poor positioning of the implant. Visual and tactile information can be critical for the surgeon to perform a technically sound TKA, including selecting the proper implant, making accurate bone cuts, and accurately aligning the implant. When these technical aspects of a TKA are less than ideal, there is an increased risk of revision due to mechanical failures of the TKA.20
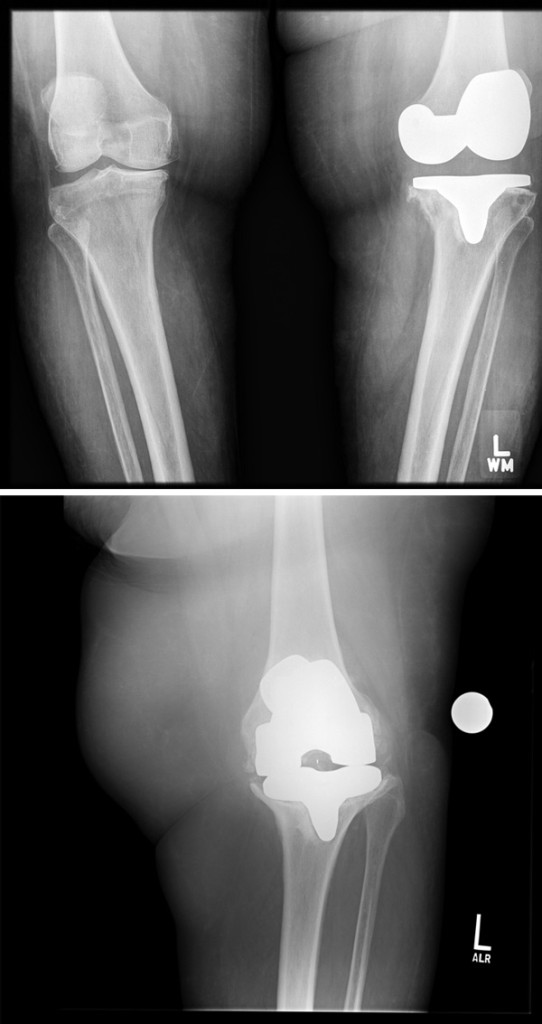
The primary mechanical failure mechanism of TKA is loosening of the implant from the bone or the cement placed around the implant during surgery.21 Although failure of TKA due to loosening is possible in any patient, those patients with elevated BMIs are at a higher risk.22 Figure 2 shows two radiographic images of an aseptically loose tibial implant in a morbidly obese patient.
The evidence assessing the impact of BMI on implant survivorship or revision rates is mixed. There are studies that report no statistical difference in the survivorship or revision rate between obese and nonobese TKA patients.23-25 However, there is evidence suggesting higher rates of revision surgery among morbidly obese TKA patients.25,26 Spicer et al compared a cohort of nonobese patients (BMI < 30) to a cohort of obese patients (BMI > 30) and found no difference in implant survivorship at 10 years.23 Bordini et al compared complication rates among nonobese patients, overweight patients, obese patients, and morbidly obese patients and found no statistical difference in the proportion of patients from these groups requiring revision.24 With the exception of the morbidly obese group, the revision rates were between 1.85% (overweight) and 1.96% (normal weight).24 The revision rate for the morbidly obese group was slightly higher at 2.3%.24
Restricted access
Because of the increased risks of complications, it is common practice for some surgeons to restrict the use of TKA in patients with a BMI of 40 or higher. Based on the current available data, many surgeons and surgeon groups across the country withhold surgical intervention in morbidly obese patients until body weight is optimized and associated medical comorbidities are better controlled.3 There may always be exceptions to this type of policy, and opponents to this position do exist. Nevertheless, the medical and societal implications of withholding TKA in morbidly obese patients are unknown.
We posit three potential outcomes for patients who are denied TKA based on their having a BMI of 40 or higher and other associated comorbidities: 1) The patient chooses to seek a second opinion and have total joint arthroplasty performed at another institution. 2) The patient chooses to seek appropriate medical options such as medical weight management counseling, bariatric surgery, or both, and achieves successful weight reduction to meet the total joint arthroplasty healthy BMI threshold (BMI less than 40). 3) The patient chooses to seek appropriate medical options such as medical weight management counseling and/or bariatric surgery, but is unable to achieve successful weight reduction to meet the total joint arthroplasty healthy BMI threshold.
We propose that this last group of patients is the cohort that is most concerning and may benefit most from a targeted care pathway and a multidisciplinary medical weight loss management team. This healthcare team should include an orthopedic surgeon, bariatric surgeon, registered dietitian, exercise specialist, and mental health provider who can in concert provide comprehensive support for the morbidly obese patient to safely achieve the target body weight and BMI required for a safe and effective TKA that can improve quality of life. We are in the initial stages of developing such a program at our institution.
Increased awareness
Recently, the American Medical Association officially categorized obesity, defined as a BMI of 30 or higher, as a disease.27 Proponents of the decision believe this move will encourage physicians to pay closer attention to obesity and enhance their patient counseling methods. Opponents suggest that the measure that is used to define obesity, i.e., BMI, is flawed.27 A patient with a considerably elevated BMI can be perfectly healthy, while a patient with a moderately elevated BMI may have related metabolic disorder and a number of associated comorbid conditions that increase the risk of complications.3,14 Therefore, opponents suggest that changing the categorization of obesity from a condition to a disease will have little impact.27 Nevertheless, the increased awareness of obesity as a public health concern can only help those who seek a healthy way to decrease their body weight and BMI,27 particularly those who are candidates for TKA.
Susan M. Odum, PhD, is the senior research scientist and outcomes research manager for the OrthoCarolina Research Institute in Charlotte, NC, and serves as part-time associate graduate faculty in the College of Health and Human Services at the University of North Carolina at Charlotte. Bryan D. Springer, MD, specializes in total joint replacement surgery at the OrthoCarolina Hip and Knee Center, where he is fellowship director.
1. Organization TWH. 10 Facts About Obesity. World Health organiation wensite. http://www.who.int/features/factfiles/obesity/facts/en/index.html. Accessed January 22, 2014.
2. Mason EE, Doherty C, Maher JW, et al. Super obesity and gastric reduction procedures. Gastroenterol Clin North Am 1987;16(3):495-502.
3. Workgroup of the American Association of Hip and Knee Surgeons Evidence Based Committee. Obesity and total joint arthroplasty: a literature based review. J Arthroplasty 2013;28(5):714-721.
4. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307(5):491-497.
5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009-2010. NCHS Data Brief 2012;(82):1-8.
6. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011-2012. NCHS Data Brief 2013;(131):1-8.
7. Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009;467(10):2606-2612.
8. Odum SM, Springer BD, Dennos AC, Fehring TK. National obesity trends in total knee arthroplasty. J Arthroplasty 2013;28(8 Suppl):148-151.
9. Fehring TK, Odum SM, Griffin WL, et al. The obesity epidemic: its effect on total joint arthroplasty. J Arthroplasty 2007;22(6 Suppl 2):71-76.
10. Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States— no change since 2003-2004. NCHS Data Drief. 2007;(1):1-8.
11. Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol 1988;128(1):179-189.
12. Coggon D, Reading I, Croft P, et al. Knee osteoarthritis and obesity. Int J Obes Relat Metab Disord 2001;25(5):622-627.
13. Gandhi R, Wasserstein D, Razak F, et al. BMI independently predicts younger age at hip and knee replacement. Obesity 2010;18(12):2362-2366.
14. Yeung E, Thornton-Bott P, Walter WL. Patient obesity: a growing concern of successful total knee arthroplasty. Semin Arthroplasty 2010;21(2):87-91.
15. Pottie P, Presle N, Terlain B, et al. Obesity and osteoarthritis: more complex than predicted! Ann Rheum Dis 2006;65(11):1403-1405.
16. Gillespie GN, Porteous AJ. Obesity and knee arthroplasty. Knee 2007;14(2):81-86.
17. Collins RA, Walmsley PJ, Amin AK, et al. Does obesity influence clinical outcome at nine years following total knee replacement? J Bone Joint Surg Br 2012;94(10):1351-1355.
18. Nunez M, Lozano L, Nunez E, et al. Good quality of life in severely obese total knee replacement patients: a case-control study. Obes Surg 2011;21(8):1203-1208.
19. Järvenpää J, Kettunen J, Kröger H, Miettinen H. Obesity may impair the early outcome of total knee arthroplasty. Scand J Surg 2010;99(1):45-49.
20. Dorr LD, Boiardo RA. Technical considerations in total knee arthroplasty. Clin Orthop Relat Res 1986;(205):5-11.
21. Schroer WC, Berend KR, Lombardi AV, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. Sep 2013;28(8 Suppl):116-119.
22. McElroy MJ, Pivec R, Issa K, et al. The effects of obesity and morbid obesity on outcomes in TKA. J Knee Surg 2013;26(2):83-88.
23. Mulhall KJ, Ghomrawi HM, Mihalko W, et al. Adverse effects of increased body mass index and weight on survivorship of total knee arthroplasty and subsequent outcomes of revision TKA. J Knee Surg 2007;20(3):199-204.
24. Spicer DD, Pomeroy DL, Badenhausen WE, et al. Body mass index as a predictor of outcome in total knee replacement. Int Orthop 2001;25(4):246-249.
25. Bordini B, Stea S, Cremonini S, et al. Relationship between obesity and early failure of total knee prostheses. BMC Musculoskelet Disord 2009;10:29.
26. Foran JR, Mont MA, Etienne G, et al. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am 2004;86-A(8):1609-1615.
27. Pollack A. AMA recognizes obesity as a disease. The New York Times. June 18, 2013. http://www.nytimes.com/2013/06/19/business/ama-recognizes-obesity-as-a-disease.html. Accessed January 22, 2014.











Hi my name is Samantha I’m 47 years old I weigh 250 pounds I need a total knee replacement and I’m looking for a doctor to do it here in Charlotte North Carolina I’m on Medicaid and I need someone to do it right away before my Medicaid runs out