 Limb length discrepancies (LLDs) as small as 1.5 cm can significantly affect gait, and some clinicians choose to intervene in cases of even smaller discrepancies. Many LLDs can be addressed orthotically, but surgical techniques are becoming less invasive and more effective.
Limb length discrepancies (LLDs) as small as 1.5 cm can significantly affect gait, and some clinicians choose to intervene in cases of even smaller discrepancies. Many LLDs can be addressed orthotically, but surgical techniques are becoming less invasive and more effective.
By Cary Groner
An old Scottish myth has it that the wild haggis—a small fictional creature typically rendered as something like a cross between an electrified hedgehog and Phyllis Diller—comes equipped with legs that are longer on one side than the other. The asymmetry helps it circumambulate the steep mountainsides of its native terrain, if only in one direction, goes the tale.
It’s an amusing concept, but unfortunately there’s a nonmythical human corollary: Leg-length discrepancies (LLDs) afflict a variety of people, including children with cerebral palsy, people who’ve had hip replacements, and those with scoliosis, pelvic obliquity, or certain muscle contractures.
According to some studies, LLDs are quite common—they’ve been reported in more than 90% of schoolchildren,1 and nearly half of athletes may have some degree of discrepancy2—but most of these cases don’t lead to symptoms. More severe LLDs, by contrast, may be associated with complications that include weakness, nerve injury, joint stiffness or dislocation, chronic pain, and arthritis.3
Research has quantified some of the effects of LLDs. In one study, for example, the authors reported that, when LLDs were artificially imposed on 44 older adults by applying platforms of varying thicknesses to one of their feet, they experienced significant quadriceps fatigue in the longer limb, and the applied LLDs caused walking difficulty beginning at 2 cm.4 Similarly, a recent article in Gait & Posture reported that, when 19 healthy individuals wore sandals of varying thicknesses to give them a discrepancy of 1.45 cm, the LLD affected pelvic motion in the frontal plane despite the participants’ compensation strategies.5 Other studies have shown that LLDs are associated with standing fatigue6 and the risk of plantar fasciitis in the longer limb.7
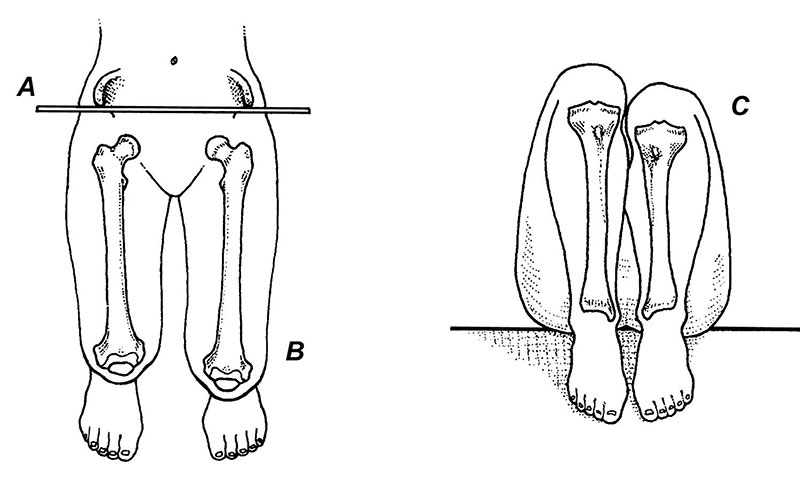
Figure 1. Allis test. The examiner manually aligns the ASIS (anterior superior iliac spine) of each limb so that they rest on the same frontal and transverse planes. The medial malleoli are then placed together, and femoral lengths are evaluated from above (left), while tibial lengths are deter- mined by comparing the levels of the tibial plateaus (right). (Reprinted with permission from reference 10.)
Although a discrepancy that may not cause symptoms for one person may lead to severe problems in another, researchers have reported that an LLD surpassing 2 cm (roughly 3/4 inch) leads to significant gait asymmetry.8 In practical terms, such asymmetries mean that the longer leg bears more weight for more time, with cumulative effects that may include increased risk of hip or knee osteoarthritis.3 Because of the potential for such negative outcomes, some clinicians intervene when LLDs are as small as 1/8 inch, particularly if the patient is an athlete.2
People with LLDs tend to compensate with tactics that help equalize functional leg length and minimize the excursion of the center of gravity, hence reducing energy cost; these include holding the foot in some degree of equinus on the shorter side, short-side pelvic drop, flexion of the knee or pronation of the foot on the longer side, or supination of the foot on the shorter side.3
Assessment
Assessment of LLDs and their effects is complicated, partly because there’s more than one type of discrepancy. Structural LLDs involve a femur or tibia that is literally shorter on one side than the other; this often leads to a tilted pelvis and related spinal complications such as scoliosis. Functional LLDs often result from pelvic obliquity related to muscle contractures or other causes; as the pelvis rotates, the legs are pulled into different apparent lengths even if the actual lengths of the bones are equal.2
Moreover, some LLDs result from a combination of structural and functional causes. One way to distinguish causative factors is to seat the patient; if the LLD is causing the scoliosis, the latter will disappear. If the scoliosis or pelvic obliquity is causing the LLD, by contrast, it will persist when the patient sits.2
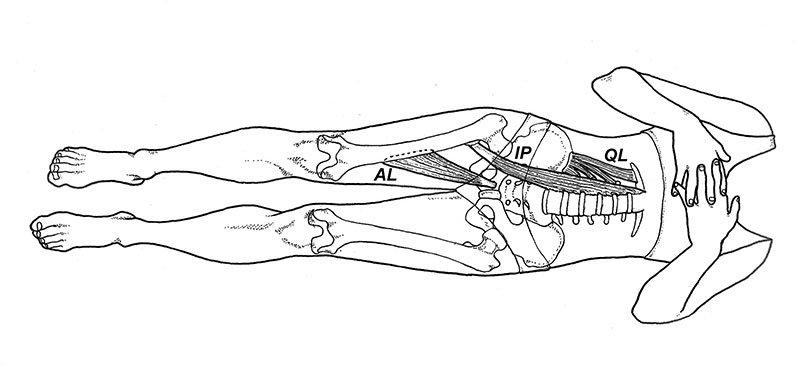
Figure 2. Functional limb-length discrepancy. Contracture of the quadratus lumborum (QL), iliopsoas (IP), and/or adductor longus (AL) muscles frequently results in a functionally shortened limb. (Reprinted with permission from reference 10.)
Structural LLDs can have multiple causes, according to Anil Bhave, PT, director of the Wasserman Gait Laboratory at the Rubin Institute for Advanced Orthopedics in Baltimore, MD.
“A child may be born with a congenital discrepancy,” Bhave said. “Growth may also be arrested due to infection or injury, which constitutes a developmental discrepancy. Finally, post-traumatic discrepancies occur when the bone shortens due to a fracture.”
Elaine Owen, MSc, MCSP, a pediatric physical therapist at the Child Development Center in Bangor, North Wales, UK, works primarily with children who have cerebral palsy (CP), spina bifida, and other hereditary disorders including sensory motor neuropathies, all of which may lead to LLDs. Such kids seem particularly susceptible to the developmental issues associated with neurological pathology.
“The trick is to find out what, exactly, is short,” Owen said. “Some children will have a short femur, a short shank, or both—sometimes with scoliosis, sometimes without. Children with these disabilities can’t compensate the way neurologically intact adults do. If you’re grown, and you have a hip replacement or a traumatic accident, one limb may become short, but neurologically you’re sound; you may use compensations such as pelvic obliquity to equalize the leg-length discrepancy. But, for children with disabilities, these compensations—knee flexing, pronating, supinating, making ground contact with an equinus foot instead of with the heel—are big problems. The debate is about when to intervene.”
Research has described some of the problems that particularly afflict children with CP. In one study, for example, the authors reported both an increased pelvic tilt range and pelvic retraction in roughly 61% of patients, and noted that factors such as LLD contributed to the deviations. They recommended that evaluation of gait abnormalities in such children should not be limited to sagittal plane kinematics but should include 3D kinematics of the pelvis as well.9
Tom Michaud, DC, a chiropractor in Newton, MA, who has written extensively about leg-length discrepancies,10 has developed a practical assessment protocol (Figures 1 and 2) that works for most of his patients. To compare tibial lengths, he has the patient recline and put the medial malleoli together. Evaluating femoral length is more challenging, he said, because tightness in certain muscles such as the quadratus lumborum can affect pelvic tilt and apparent leg length.
There may also be issues in the ankle or foot.

Figure 3. Pelvic rotation as a determinant of gait. A lateral view of the gait cycle with the knees and hips locked illustrates how the pathway of the center of mass creates an exaggerated sine wave, which is metabolically expensive because the hip abductors must raise and lower the center of mass through the exagerrated ranges. This type of sine wave pattern is more characteristic of a structural limb-length discrepancy than a functional one. (Adapted with permission from reference 10.)
“If I identify a tibial discrepancy, I’ll do a standing test and compare the heights of the medial malleoli,” he explained. “If one is lower to the ground, then I know there’s a subtalar or midtarsal component.”
Michaud said that to distinguish structural from functional LLDs he often assumes a functional discrepancy and assesses the patient’s response to stretching.
“I have them stretch the quadratus lumborum, stretch the adductors, stretch asymmetric muscle tension and see if that reduces the discrepancy,” he said. “You may also notice that almost all people with an LLD prefer to stand with more weight on the short leg, so I can note that while I’m getting their history.”
Michaud told LER that structural LLDs usually affect gait differently than functional ones, and assessing the movement of the patient’s center of mass can help distinguish the two (Figure 3).
“In a structural discrepancy, the center of mass goes high when the long leg is in midstance,” he said. “Then they drop down and will sometimes toe out on the short leg because they get a little lateral displacement of their center of mass. In a functional discrepancy, the soft tissues adapt, and you don’t see big fluctuations in the sine-wave motion of the pelvis.”
When to treat
For Michaud, decisions about what patients to treat, and how, depend on several factors.
“If someone has a chronic pain pattern—say, long-leg hip abductor pain, chronic lumbosacral pain aggravated by walking but OK with sitting, or if they’re a runner, I’ll be much more likely to address even a small structural discrepancy of, say, four millimeters,” he explained.
Typically, Michaud will give patients a heel lift, then videotape them walking. In the best cases, he sees a smoothing of pelvic motion as the patient transitions from double- to single-limb support.
The decision to prescribe an orthosis versus a heel lift depends on similar biomechanical factors, Michaud said.
“If a dropped malleolus or an asymmetric pronation is producing the leg-length discrepancy, I use an orthotic,” he said.
To assess the midtarsal component of an LLD, he employs a method he has developed that measures the change in the horizontal position of the medial malleolus as the patient moves from a talonavicular-neutral position to relaxed calcaneal stance.10
“I look for asymmetry in that medial movement component,” Michaud said. “If there’s excessive motion, patients have more medial drift on that side.”
Michaud emphasized that he never treats functional LLDs with lifts or orthoses.
“In those cases, you mobilize them, stretch them, do some muscle work, and it disappears,” he said.
Indeed, another clinician has written that, when patients with functional LLDs and scoliosis sought chiropractic treatment, in many cases the scoliosis disappeared.2
For Elaine Owen’s children with CP and other pediatric patients, intervention in LLDs may involve surgery.
“In the UK, the threshold for surgical correction is usually two centimeters by the time they’re a teenager,” she said.
Consultants measure the discrepancy with a CT scan, then assess bone age with an x-ray (children with such conditions often have a bone age different than their chronological age). Once such measurements have been done, physicians calculate when and how to intervene.
“They usually do an epiphysiodesis—a stapling of the growth plates at either the distal or proximal end of the tibia or femur of the longer leg, to stop growth,” Owen said.
There’s been some debate over decisions only to partly correct LLDs in such pediatric patients, she explained, because some surgeons prefer to leave a leg with drop foot slightly shorter to help prevent tripping in swing phase.
“The issue is whether it’s better to fully correct or not,” Owen said. “A cerebral palsy child with hemiplegia may look like they have a drop foot, but sometimes it’s just that they make initial ground contact at the end of the gait cycle with their toes. If you insert a wedge to compensate for leg length, they may make contact with their heel instead, because they were actually just trying to find the floor. So you have to consider whether you’re dealing with genuine drop foot; if you equalize leg length, do they have enough dorsiflexion capability to make initial ground contact with the heel? If so, fully correcting the leg-length discrepancy may be a good idea, rather than leaving the leg with drop foot a bit short.”
Equalizing leg lengths—whether surgically or with a heel wedge or orthosis—is important for such children for other reasons as well, including their unique compensation strategies, Owen explained.
“One common compensation is that in terminal stance they flex the longer leg to help find the floor. They can also overpronate the long leg and supinate the shorter one. So, when we have a child with a disability and a leg-length discrepancy of more than five millimeters, we almost always treat it with either footwear or AFOs [ankle foot orthoses],” she said. “Some people say you don’t need to do that, but we’ve found that it makes a big difference in how they walk. We could be more analytical about who should have a leg-length discrepancy equalized rather than assuming that all initial contacts with a toe are due to a drop foot.”
Bone growth

Figure 4. An adjustable intramedullary nail ac- tivated by an external magnet (right) offers an alternative to external fixation (left) for surgical limb lengthening. (Photo courtesy of John Herzenberg, MD.)
Surgeons tend to be cautious about the degree of correction in such cases for a variety of reasons, however. Michael Sussman, MD, a pediatric orthopedic surgeon at Shriner’s Hospital for Children in Portland, OR, told LER that his pediatric patients with leg-length
discrepancies include those with CP, vascular malformations, growth-plate infections or fractures, trauma, or idiopathic causes.
“We do our best to project patients’ bone growth, but such projections aren’t perfect,” Sussman said. “You certainly don’t want to overcorrect anyone.”
To measure patients’ bone lengths, Sussman and his colleagues use a digital dual-plane x-ray system that provides better images at a lower dose of radiation than standard radiographs. He considers patients to be candidates for lengthening surgery if the projected leg-length discrepancy will be more than four or five centimeters.
“In other cases, we can stop growth in the longer leg at the growth plates at either the distal femur or the proximal tibia, or both,” he said. “We now use screws [in the growth plates] instead of staples because you can do it through a tiny incision and they don’t have to be removed.”
Kristie Bjornson, PT, PhD, a pediatric physical therapist at Seattle Children’s Research Institute, told LER that some pediatric orthopedic surgeons may balk at lengthening children’s legs because they don’t see the results of those decisions when the children grow up.
“If you have cerebral palsy, and you grow up walking around with an asymmetrical pelvis, you’re putting stress on joints that are already stressed because of neuromuscular problems,” Bjornson said. “You end up with asymmetries, back problems, and pain; so from my perspective, treating those kids is preventive medicine. You don’t need to add leg-length discrepancies to the challenges they already have with motor control. If you correct them—whether surgically or with lifts or orthoses—their gait symmetry improves, and if you improve symmetry you improve efficiency.”
Surgeons performing leg-lengthening procedures—in adults, adolescents, and older children— have new tools at their disposal that, as they become more widespread, have the potential to significantly improve traditional fixation techniques. The old approach, known as Ilizarov distraction osteogenesis, involves wires attached to the bone from external fixators (the original wires were bicycle spokes, in fact). It’s effective but painful, and it carries infection risks.
At Sinai Hospital in Baltimore, Chief of Orthopedics John Herzenberg, MD, uses a device (Figure 4) that consists of an adjustable intramedullary nail activated by an external magnet (see “Early outcomes support internal technique for limb lengthening,” LER: Pediatrics, May 2014, page 7). (Herzenberg is an advisor to the manufacturer but receives no royalties.)
“The device is accurate, controllable, and reversible,” Herzenberg said. “I typically program it for a millimeter of growth a day, but if you want to back up a little and let the bone take a rest, you can.”
Although Herzenberg and his colleagues use the device in children as young as about 9 years, most of his patients are adults who have suffered traumatic injury or congenital deficiencies that were never treated. Not only does the approach reduce infection risk—no wires pierce the skin—the absence of external fixation makes physical therapy much easier, he said. Surgeons remove the intramedullary nail about a year after lengthening is complete, because the internal magnet would prevent future magnetic resonance imaging procedures if the patient needed them.
Herzenberg and his colleague, Anil Bhave, have documented improvements in gait parameters after leg lengthening using older techniques. In 1999, they reported in the Journal of Bone and Joint Surgery that the procedure restored stance-time symmetry in 16 of 18 patients and offered other benefits, including back pain relief.3
Restoration hardware
One source of leg-length discrepancy that’s attracted the attention of clinicians is total hip arthroplasty (THA), partly because postoperative discrepancies are a significant cause of patient dissatisfaction and litigation.11 According to the literature, the problem occurs after up to 27% of THAs.12
In many cases, LLDs that persist months after THA can be effectively managed with heel lifts or insoles; in one study, roughly two-thirds of patients with LLDs after THA found that orthotic devices were effective for symptom management.13 But a surgeon’s approach can go a long way toward minimizing the risk of these types of postoperative LLDs.
According to Peter Sculco, MD, attending surgeon in adult reconstruction and joint replacement at the Hospital for Special Surgery in New York, surgeons must take great care in measuring leg lengths while planning for a THA. True limb length is measured from the anterior superior iliac spine to the medial malleolus, whereas apparent length is measured from the umbilicus to the medial malleolus. The former measures just what it says it does; the latter considers factors that contribute to length discrepancies, such as pelvic tilt.14
“Everything starts with taking a good history,” Sculco said. “You want to identify any risk factors for a leg-length discrepancy more than the cartilage the patient will have lost from having arthritis. That’s usually about three millimeters, but most patients don’t notice because it’s happened so gradually over time, and that’s what you’re restoring when you do the reconstruction. Those other risks include pelvic obliquity that may result from either a soft-tissue contracture around the hip or from deformities in the lumbar spine.”
Once the surgeon has taken the history and made such assessments, he or she compares these findings with radiography results, Sculco explained. Pelvic reference points include the inferior aspect of the obturator foramen, the ischial tuberosities, and the acetabular teardrop.14
“You measure that fixed point on the pelvis to one on the femur, usually the lesser trochanter,” Sculco said. “You compare the two and get a radiographic difference in leg length, and hopefully that matches what you see clinically. You can then start with your templating—how you want to restore leg length at the time of surgery.”
Surgically restoring the true center of rotation of both the acetabulum and the femur should lead to restoration of the original limb length before there was arthritis-related cartilage loss, according to Sculco; that, rather than lengthening per se, is the goal.
“Let’s say you have a functional leg-length discrepancy involving a pelvic tilt, a soft-tissue contracture, that makes the operative leg a centimeter shorter,” Sculco said. “You don’t go in and lengthen the leg to eliminate the functional discrepancy, because once you put in the new hip they’re going to straighten out. They’ll lose the flexion contracture, and their pelvis will normalize over time.”
In the rare cases in which a patient has a fixed pelvic obliquity (eg, lumbar fusion) that will prevent the pelvis from naturally correcting postoperatively, surgeons may consider a planned lengthening of the leg, according to Sculco. There are other complicating factors to consider, however.
“You have to get the soft-tissue tension required for the hip not to dislocate,” he said. “Dislocation is much more catastrophic than a couple of millimeters of discrepancy. But, if you have good x-rays, valid templating, and a solid plan for restoring leg length, you should be able to get within three millimeters ninety percent of the time.”
As surgeons and other clinicians collaborate to achieve the best outcomes for the wide spectrum of patients with leg-length discrepancies, careful planning will ideally become the norm in both surgical and nonsurgical approaches to the problem, to the great benefit of patients.
Cary Groner is a freelance writer in the San Francisco Bay Area.
- Rea G, Casner V, Denslow J, et al. Progressive structural study of school children. J Am Osteopath Assoc 1951;51(3):155-157.
- Subotnick SI. Limb length discrepancies of the lower extremity (the short leg syndrome). J Orthop Sports Phys Ther 1981;3(1):11-16.
- Bhave A, Herzenberg J. Improvement in gait parameters after lengthening for the treatment of limb length discrepancy. J Bone Joint Surg Am 1999;81(4):529-534.
- Gurney B, Mermier C, Robergs R, et al. Effects of leg length discrepancy on gait economy and lower-extremity muscle activity in older adults. J Bone Joint Surg Am 2001;83(6):907-915.
- Resende RA, Kirkwood RN, Deluzio KJ, et al. Biomechanical strategies implemented to compensate for mild leg length discrepancy during gait. Gait Posture 2016;46:147-153.
- Swaminathan V, Cartwright-Terry M, Moorehead JD, et al. The effect of leg length discrepancy upon load distribution in the static phase (standing). Gait Posture 2014;40(4):561-563.
- Mahmood S, Huffman LK, Harris JG. Limb-length discrepancy as a cause of plantar fasciitis. J Am Podiatr Med Assoc 2010;100(6):452-455.
- Kaufman KR, Miller LS, Sutherland DH. Gait asymmetry in patients with limb-length inequality. J Pediatr Orthop 1996;16(2):144-150.
- Salazar-Torres JJ, McDowell BC, Kerr C, Cosgrove AP. Pelvic kinematics and their relationship to gait type in hemiplegic cerebral palsy. Gait Posture 2011;33(4):620-624.
- Michaud T. Human locomotion: The conservative management of gait-related disorders. Newton, MA: Newton Biomechanics; 2012.
- Maloney WJ, Keeney JA. Leg length discrepancy after total hip arthroplasty. J Arthroplasty 2004;19(4, suppl 1):108-110.
- Desai AS, Dramis A, Board TN. Leg length discrepancy after total hip arthroplasty: a review of the literature. Curr Rev Musculoskelet Med 2013;6(4):336-341.
- Akinola B, Jones HW, Harrison T, Tucker K. Shoe raises for symptomatic leg length discrepancy after total hip replacement: do patients find them useful? Int J Orthop Surg 2104;22(1).
- Sculco P, Cottino U, Abdel M, Sierra R. Avoiding hip instability and limb length discrepancy after total hip arthroplasty. Orthop Clin North Am 2016;47(2):327-334.









Great article. I am looking for treatment for my daughter. Please can you contact me. Thankyou
Great read, thanks!
Interesting you mentioned that surgeons “don’t see the results of those decisions when the children grow up.”
Surely some sort of followup assessments would be hugely valuable.
I had the Llizarov surgery 20 years ago, and haven’t seen a specialist for probably 17 years. I tried to get an appointment (in New Zealand), but was denied an appointment to even talk to someone… I just wanted to talk to someone about the pain I’m having now (at age 34), and see if there’s anything more I can be doing to improve my quality of life and not become a burden on society.
Beyond the quality of life and future cost to society, surely some standardized followup would be important.
My length discrepancy was around 11cm, now it seems to be around 4cm.
If anyone has any suggestions, I’m open to trying anything!..
Right now my best strategy seems to be daily yoga, eating right, orthotics, not sitting too long, massage, meditation, swimming… I’ve avoided medication so far, but had to start on intense painkillers during lockdown.
Thanks for the article!
In different accidental falls during the past four years I fractured both deniers very close to my hip. Both fractured were treated by inserting metal devices in the broken demure. I now am suffering from pain in my right hip!
I believe I need a well-designed insert in my shoe (s)designed to correct the LLD. Is there a good specialist in the Toledo/Ann Arbor area who can help me? Results to date have not worked. I am a widower who lives alone and need to get rid of my current hip pain.