 Pittsburgh researchers found that patients with diabetes have higher complication rates than nondiabetic patients following open surgical management of ankle fractures, but also that the rate of major complications in the diabetic patients was relatively low.
Pittsburgh researchers found that patients with diabetes have higher complication rates than nondiabetic patients following open surgical management of ankle fractures, but also that the rate of major complications in the diabetic patients was relatively low.
By Robert W. Mendicino, DPM, FACFAS; Alan R. Catanzariti, DPM, FACFAS; Brian Dix, DPM; and Phillip Richardson, DPM
The management of acute unstable ankle fractures in the diabetic patient can present a clinical dilemma. According to the most recent National Diabetes Fact Sheet from 2011, approximately 25.8 million people (8.3%) in the US have been diagnosed with diabetes, with 26.9% of this group aged 65 years and older.1
Diabetic patients are clearly at risk for significant lower extremity complications. The risk of infection, ulceration, and limb loss associated with the diabetic foot has been well documented.2-7 The increased risk of serious complications in the diabetic patient has been attributed to many factors, including peripheral neuropathy, nephropathy, peripheral vascular disease (PVD), impaired immune response, and delayed healing.3-8 There are also numerous studies documenting risk factors, clinical findings, and treatment guidelines for soft tissue and bone infection in the diabetic foot.2,7
The literature evaluating surgical and nonoperative treatment of ankle fractures in the diabetic patient has yielded relatively poor outcomes.2-3,7-16 The overall complication rate in diabetic patients undergoing open reduction and internal fixation (ORIF) of ankle fractures ranges from 15% to 71%.2-3,7-17 By comparison, complication rates in nondiabetic patients range from 7% to 19%.2-3,9-16 Nonoperative treatment of diabetic ankle fractures does not decrease the complication rate compared with surgical management, and, in fact, may result in a higher overall complication rate. In their classic articles Connolly3 and Leith et al14 reported complication rates of 67% and 71%, respectively, in diabetic ankle fractures that were treated nonoperatively. The complications included infection, malunion, Charcot deformity, and amputation. In the current literature, the amputation rate following surgically treated diabetic ankle fractures ranges from 0% to 20% and the development of Charcot arthropathy ranges from 0% to 50%.2-3,9-17

Anteroposterior (A/P) ankle radiograph (far left) and lateral ankle radiograph (center left) of a right trimalleolar ankle fracture. A/P ankle radiograph (center right) and lateral ankle radiograph (far right) show the same ankle after open reduction and internal fixation (ORIF).
Recently, Wukich et al8 retrospectively evaluated the outcomes of uncomplicated versus complicated operatively treated diabetic ankle fractures. Complicated ankle fractures are defined as those occurring in diabetic patients with PVD, renal disease, peripheral neuropathy, or a combination of these; uncomplicated ankle fractures occur in the absence of those conditions.10,16 They found complicated fractures were more than three times likelier to involve overall and noninfectious complications and had a five-times higher risk of the need for revision surgery than uncomplicated diabetic ankle fractures.8
We have regularly treated unstable foot and ankle fractures with operative management in the medically stable diabetic population. This paper presents an analysis of the demographics and outcomes of unstable ankle fractures treated with ORIF in the adult diabetic population compared with the nondiabetic population, and proposes a perioperative treatment protocol for management of unstable diabetic ankle fractures.
Methods
The Western Pennsylvania Hospital Institutional Review Board, West Penn Allegheny Health System, in Pittsburgh, approved this retrospective case-control clinical study. All medical and radiographic records of the 310 ankle fractures that required ORIF from 1997 to 2005 were reviewed comprehensively. Demographic and outcome data were recorded. Demographic data included age, gender, weight, medical history of diabetes, diabetes treatment, smoking, PVD, peripheral neuropathy, renal disease, inflammatory arthropathy, time to surgical treatment, and ankle dislocation. Additionally, all radiographs (anteroposterior, mortise, and lateral views) were reviewed, and ankle fracture type was determined using the Lauge-Hansen classification system.19
 Diabetes type was divided into noninsulin-dependent diabetes mellitus (NIDDM) and insulin-dependent diabetes mellitus (IDDM). Diabetes treatment types included diet only, oral agents only, oral agents plus insulin, and insulin alone. PVD was defined as previously documented PVD on admission or absent pedal pulses on physical exam. Peripheral neuropathy was defined as previously documented peripheral neuropathy or absent or diminished protective sensation via 5.07-g monofilament on exam. Renal disease was documented by treatment type, including medical treatment, hemodialysis, or renal transplant. Unstable ankle fractures requiring closed reduction in the emergency department were also identified. Complicated diabetes was defined as diabetes in conjunction with PVD, peripheral neuropathy, renal disease, or a combination of these. Uncomplicated diabetes was categorized as diabetes without any of these conditions.
Diabetes type was divided into noninsulin-dependent diabetes mellitus (NIDDM) and insulin-dependent diabetes mellitus (IDDM). Diabetes treatment types included diet only, oral agents only, oral agents plus insulin, and insulin alone. PVD was defined as previously documented PVD on admission or absent pedal pulses on physical exam. Peripheral neuropathy was defined as previously documented peripheral neuropathy or absent or diminished protective sensation via 5.07-g monofilament on exam. Renal disease was documented by treatment type, including medical treatment, hemodialysis, or renal transplant. Unstable ankle fractures requiring closed reduction in the emergency department were also identified. Complicated diabetes was defined as diabetes in conjunction with PVD, peripheral neuropathy, renal disease, or a combination of these. Uncomplicated diabetes was categorized as diabetes without any of these conditions.
Exclusion criteria included previous or current Charcot arthropathy, concurrent foot fracture, and cellulitis or ulceration at presentation. Twenty-seven patients with diabetes were eligible for this study, including one patient with bilateral ankle fractures. An equal number of nondiabetic adult patients, matched as closely as possible for age and fracture type, were selected as a control group for statistical analysis.
We used the following guidelines for operative management of ankle fractures in the diabetic patient. First, closed reduction of grossly unstable ankle fractures, layered compression dressings, and splinting should be performed at patient presentation. A preoperative time period for edema reduction should be allowed prior to any surgical intervention to decrease the risk of wound-related complications in the soft tissue envelope. ORIF should be performed as soon as the soft tissues are stable and the patient is cleared medically.
 One hour prior to surgery, all closed fractures receive a dose of a first-generation cephalosporin antibiotic. Small fragment internal fixation hardware is used on all patients. Standard AO technique should be utilized with the addition of multiple syndesmotic screws for additional ligamentous stability. Intraoperative fluoroscopy is used to access reduction and placement of plate and screws. Postoperatively, all patients receive a layered compression dressing with a posterior splint and antibiotics are continued for an additional 24 hours. A modified total contact cast is administered at discharge and the patient is seen at one- or two-week intervals for cast changes and soft tissue monitoring.
One hour prior to surgery, all closed fractures receive a dose of a first-generation cephalosporin antibiotic. Small fragment internal fixation hardware is used on all patients. Standard AO technique should be utilized with the addition of multiple syndesmotic screws for additional ligamentous stability. Intraoperative fluoroscopy is used to access reduction and placement of plate and screws. Postoperatively, all patients receive a layered compression dressing with a posterior splint and antibiotics are continued for an additional 24 hours. A modified total contact cast is administered at discharge and the patient is seen at one- or two-week intervals for cast changes and soft tissue monitoring.
It is important to monitor the contralateral limb during the postoperative period. Often, the cast may cause excoriations and bruises, especially if sensory deficits secondary to neuropathy are present. The contralateral limb should be protected, particularly during sleep. It is also important to monitor and protect the contralateral extremity from complications related to excess weightbearing. The patient is in a nonweightbearing cast for six to eight weeks and then transferred to a walking boot for an additional two to six weeks. Progression to full weightbearing is initiated after both radiographic and clinical exams demonstrate fracture stability.
Outcome data were recorded, including superficial infection, deep infection, development of Charcot arthropathy, time to healed fracture, time to unassisted full weight bearing, documented patient noncompliance, nonunion, malunion, wound dehiscence, ulceration, revision surgery, surgeries related to complications, limb loss, total hospital days including those related to complications, and death. Superficial infection was defined as infection down to the dermal layer that required oral antibiotics. Deep infection was defined as infection to include subcutaneous tissue, tendon, and bone that required intravenous antibiotics. Fracture union time was determined from radiographic examination. Serial radiographs were obtained at each postoperative visit and were evaluated for bony incorporation and to assess any positional changes. Nonunion was defined as no bony formation across the fracture site more than 90 days from the original date of surgery. Patient follow up ranged from eight months to five years.
Statistical analysis was performed on the demographic and outcome data of the diabetic and the control groups. Statistical significance was defined as a p-value < .05. Separate statistical analysis was performed within the diabetic group to compare demographics and outcome.
Results
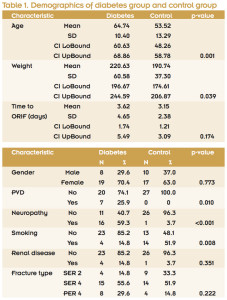
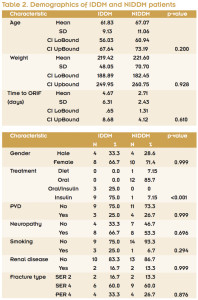
Demographic data analysis revealed that age was significantly different between the diabetic and control groups (mean age 64.74 and 53.52 years, respectively). There were eight men and 19 women in the diabetic group and 10 men and 17 women in the control group. The diabetic group’s mean weight was significantly higher than the control group’s weight (220.63 lbs vs 190.74 lbs) (p = .039). While the time to ORIF was higher in the diabetic group than the control group (3.62 days vs 2.15 days), the difference was not statistically significantly (p = .174) (Table 1). PVD was present in seven diabetic patients (25.9%) and zero control patients (p = .01). Peripheral neuropathy was found in 16 diabetic patients (59.3%, p < .001) and only one control patient. Interestingly, there were significantly more smokers in the control group than in the diabetic group (14 vs four, p = .008). Four diabetic patients and one nondiabetic patient had renal disease (p = .351). No patients in this study had a history of inflammatory arthropathy.
There was no significant difference between ankle fracture types (p = .222). Supination-external rotation type 2 (SER 2) fractures were present in four diabetic patients (14.8%) and nine control patients (33.3%). SER 4 fractures were seen in 15 diabetic patients (55.6%) and 14 control patients (51.9%). Pronation-external rotation type 4 (PER 4) fractures were present in eight diabetic patients (29.6%) and four control patients (14.8%) (Table 1). Closed reduction in the emergency department was required for 13 of 28 (46.4%) fractures in the diabetic group and nine of 27 (33.3%) in the control group, although this difference was not statistically significant (p=.412). Identical demographic comparison between the two diabetic patient types revealed that only diabetes treatment type was significantly different (p < .001) (Table 2).
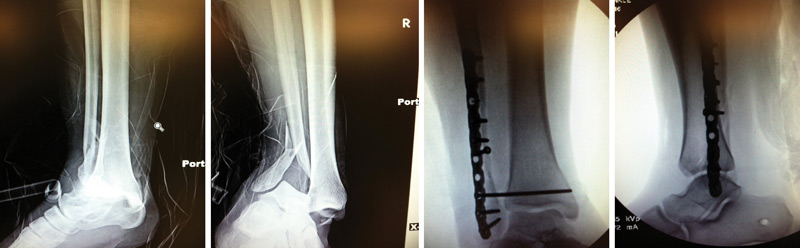
Anteroposterior (A/P) ankle radiograph (far left) and lateral ankle radiograph (center left) show of a right dislocated bimalleolar equivalent ankle fracture, prereduction. A/P ankle radiograph (center right) and lateral ankle radiograph (far right) show the same ankle immediately postop after open reduction and internal fixation (ORIF).
Outcome analysis demonstrated an overall complication rate of 32% in the diabetic group and 7% in the control group. Length of hospital stay was significantly longer for the diabetic group, 6.58 days compared with 2.17 days for controls (p <.001). Time to full weightbearing without assistance was longer for the diabetic group (11 weeks) than the control group (9.37 weeks) but the difference was not significant (p = .351). Time to fracture union was slightly longer for the diabetic group (10.96 weeks) compared with the control group (10.08), but again the difference was not statistically significant (p = .639) (Table 3). Five diabetic patients developed a wound dehiscence (17.9%), three 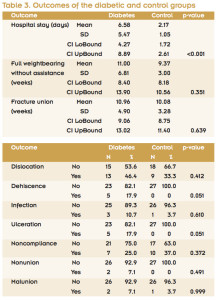 of which progressed to ulceration. Three diabetic patients had wound infections, of which two were superficial and one deep. Of the diabetic patients with infection, two went on to ulceration. One patient’s outcome was complicated by superficial infection and exposed hardware that required removal, but that patient subsequently healed without further complication. The only patient with deep infection required multiple debridements, free tissue transfer, and skin grafting to achieve wound closure. One diabetic patient with an open fracture went on to heal uneventfully. All patients with dehiscence, infection, and ulceration went on to heal. Documented noncompliance with strict nonweightbearing occurred in seven (25%) of the diabetic patients and 10 (37%) of the control patients. This difference was not statistically significant (p = .372) (Table 3).
of which progressed to ulceration. Three diabetic patients had wound infections, of which two were superficial and one deep. Of the diabetic patients with infection, two went on to ulceration. One patient’s outcome was complicated by superficial infection and exposed hardware that required removal, but that patient subsequently healed without further complication. The only patient with deep infection required multiple debridements, free tissue transfer, and skin grafting to achieve wound closure. One diabetic patient with an open fracture went on to heal uneventfully. All patients with dehiscence, infection, and ulceration went on to heal. Documented noncompliance with strict nonweightbearing occurred in seven (25%) of the diabetic patients and 10 (37%) of the control patients. This difference was not statistically significant (p = .372) (Table 3).
Two diabetic patients and zero control patients developed fracture nonunions. The only patient in the study with bilateral fractures was noncompliant with weightbearing status and developed a malunion and syndesmotic diastasis that required long-term bracing. The other diabetic patient with a nonunion went on to heal at seven months despite a history of noncompliance with weightbearing status and smoking. An additional control patient with a malunion developed a distal syndesmotic diastasis that was revised seven weeks postoperatively and went on to heal successfully.
Analysis of outcomes between the two diabetes types showed mean length of hospital stay was higher in the IDDM patients (7.82 days) versus the NIDDM patients (5.54 days), but this difference was not statistically significant (p = .320). Mean time to full weightbearing without assistance was the same (11 weeks) in both groups. Mean time to fracture union was slightly higher in the IDDM group (11.46 weeks) than the NIDDM group (10.53 weeks), but this difference was not significant (p = .550).
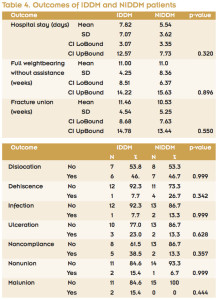 Analysis of the other outcomes revealed very similar results between the NIDDM and IDDM groups (Table 4). There were no amputations, limb loss, deaths, or cases of Charcot arthropathy during the postoperative period.
Analysis of the other outcomes revealed very similar results between the NIDDM and IDDM groups (Table 4). There were no amputations, limb loss, deaths, or cases of Charcot arthropathy during the postoperative period.
There were no statistically significant differences between the 10 uncomplicated diabetic fractures and the 18 complicated diabetic fractures for any of the outcome categories previously studied. Moreover, there was a trend (not evaluated statistically) for a higher rate of complications, longer hospital stay, and increased mean time to full weightbearing without assistance in the uncomplicated diabetes group. However, there was also a trend for more ulcerations associated with complicated diabetic fractures than uncomplicated diabetic fractures.
Discussion
Connolly and Csenscitz3 stated, “A fracture in the ankle of a patient with longstanding diabetes and neuropathy can be a calamity for the patient and the physician who treats the fracture as a routine injury.” Outcomes from the current literature confirm this statement, with relatively high rates of Charcot arthropathy and limb loss reported.2-3,9,11-14,16 However, the low rate of major complications and lack of statistically significant differences in patient outcomes in our study contradict the older published data and are more comparable to the recent published data.10,17 Costigan et al, for example, found that open fractures, insulin dependence, patient age, and fracture classification had no significant effect on outcome.
A national data bank of 160,598 adult patients was used to assess the impact of diabetes on outcomes after ankle fracture.20 Ganesh et al found significantly higher values for postoperative complications, length of hospital stay, discharge, and total charges in diabetic patients with ankle fractures than in nondiabetic patients.20 Their average length of stay for a diabetic patient was 4.7 days compared with 3.6 days in the nondiabetic group.20 Our study showed that diabetic patients on average stayed approximately five days longer in the hospital for surgical treatment of an ankle fracture than nondiabetic patients. This increased length of stay can be contributed to more rigorous medical clearance needed to minimize the comorbid conditions and possible complications that can occur following the surgery.

Anteroposterior (A/P) ankle radiograph (far left) and lateral ankle radiograph (center left) show a right trimalleolar ankle fracture, postreduction. A/P ankle radiograph (center), medial-oblique ankle radiograph (center right), and lateral ankle radiograph (far right) show the same ankle immediately postop after open reduction and internal fixation (ORIF).
It has been reported in the past that patients with diabetes sustain more severe ankle fractures than patients without diabetes.20-24 Our study is comparable to the previous published reports. Nearly half (46%) of the diabetic patients required closed reduction in the emergency department, compared with 33% of the control group. There were twice as many PER 4 fractures in the diabetic group but an almost equal number of SER 4 fractures in both groups.
This study found no significant difference in outcomes when comparing the NIDDM and IDDM patients, which is consistent with the work of Costigan et al.17 However, a study by Blotter et al found a higher complication rate in IDDM patients than in NIDDM patients, and a study by Jones et al16 reported a worse prognosis for IDDM patients than NIDDM patients after ORIF of an ankle fracture.
There was no significant difference in fracture healing time between the diabetic group and control group in this study. Loder25 and Bibbo et al2 have stated that diabetic ankle fractures heal slower than nondiabetic ankle fractures. The data from our study do not support this theory and are more consistent with Boddenberg’s published results that diabetic patients heal at only slightly slower rates than nondiabetic patients.18 Diabetic fracture healing occurred at a mean of 11 weeks as compared to 10 weeks for the control group.
Soohoo et al10 evaluated more than 57,000 operative ankle fractures using California’s discharge database and found that complicated diabetes (peripheral neuropathy, nephropathy, PVD) was a significant predictor of short-term and intermediate-term complications (odds ratio 2 to 5.65, p < .001). However, our study demonstrated only 13% of diabetic patients with peripheral neuropathy and 57% of diabetic patients with PVD developed infections and ulcerations. There were no surgical complications with the four diabetic patients with renal disease. Furthermore, there was no significant difference in complication rates between uncomplicated and complicated diabetes. The low rate of wound complications in the neuropathic population in our study could be attributed to the application of a modified total contact cast at discharge and the frequency of follow up appointments for all diabetic patients.
Bibbo et al2 advocated a 10-to-14 day waiting period after closed reduction and splinting prior to ORIF of diabetic ankle fractures. The authors felt that “significant wound complications can be minimized” if ORIF is delayed. There were six superficial infections and one deep infection in their series of 13 patients, for an infection rate of 54%. In our study ORIF was performed on average 3.62 days after diabetic ankle fracture, and the combined infection and ulceration rate was 19%. This average time included two patients who had ORIF 14 and 21 days after their fracture. Our two patients with the longest time to ORIF both developed ulcerations and one developed malunion and nonunion. We advocate early ORIF whenever possible to avoid difficulty obtaining anatomic reduction in the delayed presentation. Early ORIF of severe ankle fractures to avoid complications has been previously advocated by Carragee et al26 and Blotter et al.9 However, if edema is extensive we do recommend a waiting period.
This study did not assess internal fixation constructs and their association with complications and healing times; however, all patients in this study had ORIF performed utilizing standard AO (Arbeitsgemeinschaft für Osteosynthesefragen [Association for the Study of Internal Fixation]) principles. These included interfragmentary screw compression, lateral fibular plating, medial malleolar fixation (screws, k-wires, or tension banding) and trans-syndesmotic screw stabilization when necessary. We now advocate the use of multiple syndesmotic screws and have a lower threshold for the use of syndesmotic fixation, even in SER fracture dislocations. There were no hardware failures in our series, in contrast to the study by Blotter et al9 that reported three hardware failures with ORIF of ankle fractures in 21 diabetic patients. In a study by Jani et al,11 percutaneous transarticular fixation across the subtalar and ankle joints, in addition to standard techniques, was part of a ankle fracture standard protocol for all patients with diabetic neuropathy. Unfortunately, four of 16 patients in this series developed major complications, including two patients who required amputation following deep infection.11 We have utilized this technique of transarticular pinning in addition to standard ORIF for the management of severely unstable diabetic ankle fractures.
Bibbo et al describe a postoperative course that begins with eight weeks of nonweightbearing cast immobilization. Over the next eight to 12 weeks the patient progresses from partial weight bearing to full weight bearing with the assistance of a walking boot.2 Costigan et al began weightbearing in a short leg cast four to eight weeks following surgery and kept patients in a walking cast for an additional two to six weeks.17 Moreover, Wukich et al8 initiated eight weeks of nonweightbearing after ankle fracture in diabetic patients without peripheral neuropathy and 12 weeks of nonweightbearing in diabetic patients with peripheral neuropathy. External fixation and transarticular pins were removed at eight to 12 weeks postoperatively. Our protocol included a nonweightbearing cast for six to eight weeks, with all diabetic patients receiving a modified total contact cast. Patients were then transferred into a walking boot for an additional two to six weeks. Our diabetic patient group was fully weightbearing at an average of 11 weeks, compared with nine weeks for the control group.
Like Bibbo et al2, we excluded patients with a history of Charcot arthropathy. These patients have been shown to have higher and more serious complication rates that could limit the applicability of our analysis. Jones et al16 noted that “the comorbidity of a history of Charcot neuroarthropathy was independently associated with every complication measured” in their analysis of diabetic ankle fractures. We were fortunate to have no outcomes of Charcot arthropathy, limb loss, or death in our series. These findings differ from what has been reported in the literature.2,3,9,11,13,14,16,17,27,28
Limitations of this study include imprecise age matching between the diabetic and control groups. This could have influenced the few statistically significant findings in this study. Also, our assessment of peripheral neuropathy and PVD were based on medical history and physical exam in an emergency department setting, where factors such as pain, swelling, and apprehension could have precluded an accurate diagnosis. Limitations also include our small sample size, especially when comparing uncomplicated and complicated diabetes, and the study’s retrospective nature. However, we attempted to add strength to our statistical analysis by comparing the diabetic group to a nondiabetic control group.
Conclusion
The data from this study demonstrate that diabetic patients with ankle fractures have higher postoperative complication rates than nondiabetic patients and significantly longer hospital stays. Furthermore, our evaluation reveals a relatively low major complication rate for diabetic ankle fractures treated with open management compared to nondiabetic patients. This could partly be due to aggressive management, including total contact casting in all diabetic ankle fractures.
Robert W. Mendicino, DPM, FACFAS, is on the faculty in the Division of Foot & Ankle Surgery, West Penn Allegheny Health System in Pittsburgh, PA, and in private practice at Pinnacle Orthopedic Associates in Salisbury, NC. Alan R. Catanzariti, DPM, FACFAS, is residency director and Brian Dix, DPM, and Phillip Richardson, DPM, are residents in the Division of Foot & Ankle Surgery, West Penn Allegheny Health System.
Acknowledgement: The authors thank Janine E. Janosky, PhD, for the statistical analysis.
- Diabetes Statistics: Data from the 2011 National Diabetes Fact Sheet. American Diabetes Association website. http://www.diabetes.org/diabetes-basics/diabetes-statistics/. Published January 26, 2011. Accessed March 18, 2013.
- Bibbo C, Lin SS, Beam HA, Behrens FF. Complications of ankle fractures in diabetic patients. Orthop Clin North Am 2001;32(1):113-133.
- Connolly JF, Csencitz TA. Limb threatening neuropathic complications from ankle fractures with diabetes. Clin Orthop 1998;348(3):212-219.
- Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery: a comparison of patients with and without diabetes. Diabetes Care 2011;34(10):2211-2013.
- Holmes GB, Hill N. Fractures and dislocations of the foot and ankle in diabetics associated with Charcot joint changes. Foot Ankle Int 1994;15(4):182-185.
- Myers TG, Lowery NJ, Frykberg RG, Wukich DK. Ankle and hindfoot fusions: comparison of outcomes in patients with and without diabetes. Foot Ankle Int 2012;33(1):20-28.
- Wukich DK, Kline AJ. The management of ankle fractures in patients with diabetes. J Bone Joint Surg Am 2008;90(7):1570-1578.
- Wukich DK, Joseph A, Ryan M, et al. Outcomes of ankle fractures in patients with uncomplicated versus complicated diabetes. Foot Ankle Int 2011;32(2):120-130.
- Blotter RH, Connolly E, Wasan A, Chapman MW. Acute complications in the operative treatment of isolated ankle fractures in patients with diabetes mellitus. Foot Ankle Int 1999;20(11):687-694.
- SooHoo NF, Krenek L, Eagan MJ, et al. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am 2009;91(5):1042-1049.
- Jani MM, Ricci WM, Borrelli J Jr, et al. A protocol for treatment of unstable ankle fractures using transarticular fixation in patients with diabetes mellitus and loss of protective sensibility. Foot Ankle Int 2003;24(11):838-844.
- Kristiansen B. Ankle and foot fractures in diabetics provoking neuropathic joint changes. Acta Orthop Scand 1980;51(6):975-979.
- Low CK, Tan SK. Infection in diabetic patients with ankle fractures. Ann Acad Med Singapore 1995;24(3):353-355.
- McCormack RG, Leith JM. Ankle fractures in diabetics. Complications of surgical management. J Bone Joint Surg Br 1998;80(4):689-692.
- Kline AJ, Gruen GS, Pape HC, et al. Early complications following the operative treatment of pilon fractures with and without diabetes. Foot Ankle Int 2009;30(11):1042-1047.
- Jones KB, Maiers-Yelden KA, Marsh JL, et al. Ankle fractures in patients with diabetes mellitus. J Bone Joint Surg Br 2005;87(4):489-495.
- Costigan W, Thordarson MD, Debnath UK. Operative management of ankle fractures in patients with diabetes mellitus. Foot Ankle Int 2007;28(1):32-37.
- Boddenberg U. Healing time of foot and ankle fractures in patients with diabetes mellitus: literature review and report on own cases. Zentralbl Chir 2004;129(6):453-459.
- Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigation. Arch Surg 1950;60(5):957-985.
- Ganesh SP, Pietrobon R, Cecilio W, et al. The impact of diabetes on patient outcomes after ankle fracture. J Bone Joint Surg Am 2005;87(8):1712-1718.
- White CB, Turner NS, Lee GC, Haidukewych GJ. Open ankle fractures in patients with diabetes mellitus. Clin Orthop Relat Res 2003;(414):37-44.
- Donley BG, Philbin T, Tomford JW, Sferra JJ. Foot and ankle infections after surgery. Clin Orthop Relat Res 2001;(391):162-170.
- Marks RM. Complications of foot and ankle surgery in patients with diabetes. Clin Orthop Relat Res 2001;(391):153-161.
- Carnevale V, Romagnoli E, D’Erasmo E. Skeletal involvement in patients with diabetes mellitus. Diabetes Metab Res Rev 2004;20(3):196-204.
- Loder RT. The influence of diabetes mellitus on the healing of closed fractures. Clin Orthop Relat Res 1988;(232):210-216.
- Carragee EJ, Csongradi JJ, Bleck EE. Early complications in the operative treatment of ankle fracture: Influence of delay before operation. J Bone Joint Surg Br 1991;73(l):79-82.
- Schon LC, Easley ME, Weinfeld SB. Charcot neuroarthropathy of the foot and ankle. Clin Orthop Relat Res 1998;(349):116-131.
- Kristiansen B. Ankle and foot fractures in diabetics provoking neuropathic joint changes. Acta Orthop Scand 1980;51(6):975-979.







