 Many knee injury prevention programs do not focus on ankle dorsiflexion range of motion and hip adductor activation, but research suggests both distal and proximal variables contribute to alterations in frontal plane knee biomechanics and could affect injury risk.
Many knee injury prevention programs do not focus on ankle dorsiflexion range of motion and hip adductor activation, but research suggests both distal and proximal variables contribute to alterations in frontal plane knee biomechanics and could affect injury risk.
By Darin A. Padua, PhD, ATC, and Micheal A. Clark, DPT, MS, PES, CES
Musculoskeletal injuries from sports represent serious long-term health concerns for millions of young Americans.1 Sport and recreational injuries result in seven million physician visits each year,1 with lower extremity injuries comprising 66% of all sports injuries. The knee is the joint most commonly injured.2 Known risk factors for knee injury (e.g., anterior cruciate ligament [ACL] injury, patellofemoral pain, knee osteoarthritis, medial collateral ligament [MCL] injury, and knee cartilage/meniscus damage) include altered frontal plane biomechanics of the knee joint.3-9 Therefore, the effectiveness of knee injury prevention programs may depend on the ability to modify those neuromuscular characteristics that influence frontal plane knee biomechanics.
The hip abductor, extensor, and external rotator muscles (gluteus medius and maximus) are frequently described as critical factors controlling frontal plane knee biomechanics.10,11 Research investigating the influence of gluteal muscle activation, strength, or both on frontal plane knee biomechanics is mixed, with multiple studies showing no association between gluteal muscle function and frontal plane knee biomechanics.12-15 Therefore, other factors that influence frontal plane knee biomechanics may exist. Several recent studies indicate that limited ankle dorsiflexion ranges of motion (ROM) and hip adductor muscle activation are neuromuscular characteristics contributing to altered frontal plane knee biomechanics, and subsequent knee injury risk. The purpose of this review is to highlight the current evidence in this area of study.
Ankle dorsiflexion and knee biomechanics
Restricted ankle dorsiflexion motion is an important factor associated with altered frontal plane knee biomechanics.
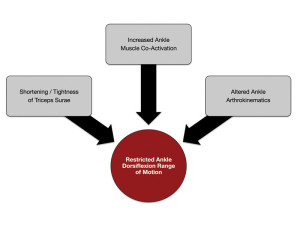
Figure 1. Restricted ankle dorsiflexion, and the accompanying changes in frontal plane knee biomechanics, may be influenced by multiple mechanisms.
Repeated studies have observed a 20% decrease in ankle dorsiflexion ROM in those who display excessive medial knee displacement (MKD), for example, dynamic knee valgus collapse, compared with those without displacement during both double-leg squat12,13,15 and single-leg squat tasks.14 In a separate study using different participants, knee varus during a double-leg squat was greater in those with restricted ankle dorsiflexion ROM.16
These collective findings indicate that limited passive ankle dorsiflexion ROM appears to be associated with an inability to maintain neutral frontal plane knee alignment. Individuals with restricted passive ankle dorsiflexion ROM display greater frontal plane knee motion that may occur in either the valgus and varus direction of motion.
These studies do not demonstrate whether restricted ankle dorsiflexion motion causes altered frontal plane knee biomechanics. To better understand if reduced ankle dorsiflexion motion causes altered frontal plane knee biomechanics, researchers manipulated the available range of ankle dorsiflexion motion during functional tasks.12,13 Researchers increased the available ankle dorsiflexion motion in those with visible MKD by placing a two-inch lift under their heels. This positioned the ankle in greater relative plantarflexion at the onset of movement, creating an increased available range of dorsiflexion motion during the squat task.
The use of a heel lift significantly reduced MKD.12,13 With the heel lift in place the MKD participants no longer demonstrated dynamic knee valgus collapse and maintained their knees over their toes. Thus, increasing the available range of ankle dorsiflexion motion resulted in an immediate improvement to frontal plane knee biomechanics.
In a separate study, researchers restricted the available range of ankle dorsiflexion motion by placing a 12° wedge under each participant’s forefoot.17 The use of the forefoot wedge placed the ankle in a more dorsiflexed position at the start of the squat task, thereby reducing the available motion. After restricting the available ankle dorsiflexion motion, the participants demonstrated a significant increase in knee valgus alignment compared the same measure without use of the wedge.17
These findings demonstrate that alterations to the available range of ankle dorsiflexion motion during functional tasks, such as squatting, cause acute alterations in frontal plane knee biomechanics. Due to the effects of ankle dorsiflexion motion on frontal plane knee biomechanics, interventions aimed to increase ankle dorsiflexion motion may be important components of an integrated knee injury prevention program.
Shortening of the gastrocnemius and soleus musculature restricts the available ankle dorsiflexion motion. In addition, ankle muscle coactivation may increase ankle joint stiffness as well as limit ankle dorsiflexion motion. Repeated studies have demonstrated increased gastrocnemius, soleus, and tibialis anterior muscle coactivation in individuals who display MKD.12,15,17 Other research demonstrates that arthrokinematic motion may be disrupted due to bony positional faults, which also leads to restricted ankle dorsiflexion motion.18-21 For example, restricted ankle dorsiflexion motion is commonly observed following lateral ankle sprains due to a decreased posterior talar glide or an anteriorly positioned fibula (proximal or distal end).
Thus, restricted ankle dorsiflexion motion, and the accompanying changes in frontal plane knee biomechanics, may be influenced by multiple mechanisms, including: 1) shortening of the triceps surae musculature, 2) increased ankle muscle coactivation, or 3) altered ankle arthrokinematics (Figure 1). Clinicians overseeing knee injury prevention programs should consider addressing all mechanisms of ankle dorsiflexion motion restriction to achieve optimal gains in the available motion and restore normal frontal plane knee biomechanics.
Ankle dorsiflexion and knee injury rates
Recent research highlights the importance of ankle dorsiflexion ROM as a risk factor for knee injury. Several retrospective studies have reported those with chronic knee pain (e.g., patella tendinopathy or patellofemoral pain syndrome) also displayed decreased ankle dorsiflexion ROM compared with healthy individuals.22-24
Using a prospective cohort study design, Backman et al demonstrated decreased ankle dorsiflexion ROM to predict future development of patella tendinopathy in volleyball athletes.25 Specifically, those with less than 36.5° of motion during the weight-bearing lunge test were more likely to develop patella tendinopathy within one year of initial testing.25
These studies provide initial evidence to support the influence of restricted ankle dorsiflexion motion on chronic knee injury risk. Future research is needed to identify whether similar relationships exist between restricted ankle dorsiflexion motion and acute knee injuries, such as noncontact ACL injury.
There are multiple mechanisms through which restricted ankle dorsiflexion motion may influence knee injury risk. As previously described, restricted ankle dorsiflexion motion alters frontal plane knee biomechanics,12-17 thus providing a mechanism for the occurrence of ACL,26 MCL,9 meniscus,27 and chronic knee injuries.6-8
Additionally, knee joint energy absorption is influenced by ankle dorsiflexion motion. Approximately 37% to 50% of the total kinetic energy is absorbed at the ankle joint as it undergoes dorsiflexion when landing from a jump.28 Individuals with restricted ankle dorsiflexion motion may have a diminished ability absorb kinetic energy at the ankle, due to the restricted available motion. This leads to compensatory increases in knee joint energy absorption, leading to greater loads on the surrounding soft tissue structures and increasing the risk of knee injury. Thus, either altered frontal plane knee biomechanics, increased knee joint energy absorption, or both are theorized to increase the risk of knee injury. As such, ankle dorsiflexion mobility training should be a key component of knee injury prevention programs.
Hip adduction and knee biomechanics
Hip adductor muscle activation may also influence frontal plane knee biomechanics,12,14,15 thus potentially influencing knee injury rates. Interestingly, Mauntel et al14 observed no difference in gluteal muscle activation in those with and without MKD during a single-leg squat. However, when examining the relative activation between the gluteal and hip adductor musculature, the coactivation ratio (gluteal activation adductor activation) was approximately 1. This indicates nearly equal hip adductor muscle activity relative to gluteal activity in the MKD group.
In contrast, those who maintained neutral alignment (no presence of MKD) had coactivation ratios of 3-4, which indicates gluteal muscle activation was three to four times greater than that of the hip adductors in these individuals.
Similar findings were reported in two research reports investigating a double-leg squat task.12,15 Both studies found no significant differences in either gluteus maximus or gluteus medius muscle activation between those with and without visual presence of MKD.12,15 However, there was significantly greater hip adductor muscle activation in the participants with MKD compared with those without the characteristic.2,15
Based on these findings, increased activation of the hip adductors appears to be an important contributor to increased MKD. Future research should continue to examine the relative activation between the gluteal and adductor muscles. This may represent a more functionally relevant way to examine the influence of muscle activation on frontal plane knee biomechanics, given that both abductors and adductors can influence frontal plane lower extremity alignment.
These findings also suggest the importance of restoring muscle balance between the hip abductors and adductors as part of a knee injury prevention program. It may be necessary to address hip adductor over-activation by incorporating techniques that lead to inhibition and relaxation of the hip adductor muscles as part of an integrated exercise strategy to restore muscle balance and minimize the hip adduction moment that may produce increased MKD.
It is worth noting that most experts think MKD is more prevalent or excessive in women than in men. Thus, it is possible that differences in ankle dorsiflexion motion and hip adductor activation in those with and without MKD may be influenced by the individual’s sex.
In the previously described studies investigating ankle dorsiflexion motion and hip adductor activation, we included both male and female participants. During the screening procedures it appeared that a larger proportion of women than men demonstrated MKD, which is consistent with previous reports. However, the number of men and women in the MKD and control groups were equivalent in these studies.
Regardless of the participant’s sex, those with MKD demonstrated less ankle dorsiflexion motion and greater hip adductor activation compared to those without MKD. Thus, while MKD does appear to be more prevalent in women, the presence of restricted ankle dorsiflexion motion and greater hip adductor muscle activation occurs in both men and women who display MKD.
Corrective exercise strategy
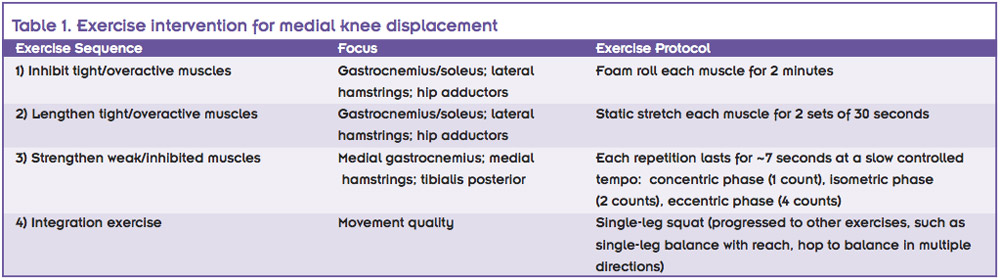
Bell et al examined the importance of improving ankle dorsiflexion ROM combined with adductor muscle relaxation and lengthening in correcting frontal plane knee biomechanics.29 In this study, all participants displayed visual presence of MKD during a double-leg squat, which was corrected when performing the squat on heel lifts. The majority of enrolled participants were women (~90%), with only three men (intervention group = 1; control group = 2). Participants were randomly assigned to a control or intervention group. The intervention group performed 10 exercises sessions over three to four weeks. The intervention program followed a four-step exercise sequence (see Table 1).
Achieving relaxation and lengthening of the gastrocnemius and soleus and hip adductor muscles to facilitate increased ankle dorsiflexion and hip abduction ROM were two major goals of the intervention.
Following the intervention period, there was a significant decrease in knee valgus motion during the double-leg squat combined with an increase in ankle dorsiflexion ROM.29 Hip adductor muscle activation and hip abduction range of motion was not assessed in this study, thus it is not known if these variables were changed following the intervention.
In contrast, nearly all of the many studies that failed to correct frontal plane knee biomechanics following an exercise intervention did not address ankle dorsiflexion and hip adduction restrictions.29 These findings highlight the importance of addressing ankle dorsiflexion and hip adduction restriction as components of an integrated training program to correct frontal plane knee biomechanics. Given the impact of increasing ankle dorsiflexion motion on MKD, future research investigating the effect of foot orthotic devices that may positively influence ankle dorsiflexion motion is warranted.
Implications for injury prevention
It is apparent that multiple factors may influence frontal plane knee biomechanics and, ultimately, knee injury risk.
We propose restricted ankle dorsiflexion motion and increased hip adductor activation are two often-overlooked components of knee injury prevention programs. Given the associations between increased MKD with restricted ankle dorsiflexion motion and increased hip adductor activation, these variables should be addressed in programs designed to improve frontal plane knee biomechanics. This is not to suggest that gluteal or core muscle strengthening are not important components for knee injury prevention. Rather, the integration of specific exercises to address all of these components (Figure 2) may be needed to optimize the programs that aim to improve frontal plane knee biomechanics by limiting MKD.
Darin A. Padua, PhD, ATC, is professor and chair of the Department of Exercise and Sport Science at the University of North Carolina at Chapel Hill. Micheal A. Clark, DPT, MS, PES, CES, is a physical therapist at Phoenix Sun in Phoenix, AZ, and founder and chief executive officer of Fusionetics in Atlanta.
1. Conn JM, Annest JL, Gilchrist J. Sports and recreation related injury episodes in the US population, 1997-99. Inj Prev 2003;9(2):117-123.
2. Hootman JM, Macera CA, Ainsworth BE, et al. Epidemiology of musculoskeletal injuries among sedentary and physically active adults. Med Sci Sports Exerc 2002;34(5):838-844.
3. Hewett TE. Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med 2005;34(3):490-498.
4. Griffin LY. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II Meeting, January 2005. Am J Sports Med 2006;34(9):1512-1532.
5. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38(10):1968-1978.
6. Elias JJ, Mattessich SM, Kumagai M, et al. In vitro characterization of the relationship between the Q-angle and the lateral component of the quadriceps force. Proc Inst Mech Eng H 2004;218(1):63-67.
7. Mizuno Y, Kumagai M, Mattessich SM, et al. Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res 2001;19(5):834-840.
8. Brouwer GM, van Tol AW, Bergink AP, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum 2007;56(4):1204-1211.
9. Hull ML, Berns GS, Varma H, Patterson HA. Strain in the medial collateral ligament of the human knee under single and combined loads. J Biomech 1996;29(2):199-206.
10. Lawrence RK, Kernozek TW, Miller EJ, et al. Influences of hip external rotation strength on knee mechanics during single-leg drop landings in females. Clin Biomech 2008;23(6):806-813.
11. Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech 2006;22(1):41-50.
12. Padua DA, Bell DR, Clark MA. Neuromuscular characteristics of individuals displaying excessive medial knee displacement. J Athl Train 2012;47(5):525-536.
13. Bell DR, Padua DA, Clark MA. Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Arch Phys Med Rehabil 2008;89(7):1323-1328.
14. Mauntel TC, Begalle RL, Cram TR, et al. The effects of lower extremity muscle activation and passive range of motion on single leg squat performance. J Strength Cond Res 2013;27(7):1813-1823.
15. Bell DR, Vesci BJ, DiStefano LJ, et al. Muscle activity and flexibility in individuals with medial knee displacement during the overhead squat. Athl Train Sports Health Care 2011;4(3):117-125. 20110817-03.
16. Dill K, Begalle RL, Frank BS, et al. Knee and ankle kinematics during squatting are altered in those with limited ankle dorsiflexion range of motion assessed during a weight bearing lunge. J Athl Train In press.
17. Macrum E, Bell DR, Boling M, et al. Effect of limiting ankle-dorsiflexion range of motion on lower extremity kinematics and muscle-activation patterns during a squat. J Sport Rehabil 2012;21(2):144-150.
18. Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther 2002;32(4):166-173.
19. Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res 2012;30(11):1798-804.
20. Hoch MC, McKeon PO. The effectiveness of mobilization with movement at improving dorsiflexion after ankle sprain. J Sport Rehabil 2010;19(2):226-232.
21. Landrum EL, Kelln BM, Parente WR, et al. Immediate effects of anterior-to-posterior talocrural joint mobilization after prolonged ankle immobilization: a preliminary study. J Man Manip Ther 2008;16(2):100-105.
22. Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther 2005;35(12):793-801.
23. Witvrouw E, Lysens R, Bellemans J, et al. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med 2000;28(4):480-489.
24. Malliaras P, Cook JL, Kent P. Reduced ankle dorsiflexion range may increase the risk of patellar tendon injury among volleyball players. J Sci Med Sport 2006;9(4):304-309.
25. Backman LJ, Danielson P. Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study. Am J Sports Med 2011;39(12):2626-2633.
26. Hewett TE. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 2005;33(4):492-501.
27. Senter C, Hame SL. Biomechanical analysis of tibial torque and knee flexion angle: implications for understanding knee injury. Sports Med 2006;36(8):635-641.
28. Devita P, Skelly WA. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sports Exerc 1992;24(1):108-115.
29. Bell DR, Oates DC, Clark MA, Padua DA. Two- and 3-dimensional knee valgus are reduced after an exercise intervention in young adults with demonstrable valgus during squatting. J Athl Train 2013;48(4):442-449.









Lot of great information for an all too common topic. My programs have injury prevention in mind and definitely the ACL especially with my female athletes. I plan on using some of the information you’ve provided about the ankle as a contributing factor. Those facts made me recall Gray Cook demonstrating ankle mobility stretches after having someone perform the FMS.