In both the short term and the long term, anterior cruciate ligament reconstruction produced greater quality of life improvements at a lower cost compared with rehabilitation only, suggesting that limiting access to ACL reconstruction may be harmful to patients and costly to society.
In both the short term and the long term, anterior cruciate ligament reconstruction produced greater quality of life improvements at a lower cost compared with rehabilitation only, suggesting that limiting access to ACL reconstruction may be harmful to patients and costly to society.
By Richard C. Mather III, MD, and Lane Koenig, PhD
One of the four ligaments within the knee, the anterior cruciate ligament (ACL) is a commonly injured knee ligament, particularly among younger physically active people. The ACL runs diagonally in the middle of the knee, preventing the tibia from sliding out in front of the femur and providing stability as the knee rotates, such as when individuals play sports like basketball, football, tennis, and soccer. An unstable knee increases the risk of injury to other important knee structures, such as the meniscus and cartilage, which leads to a higher risk of developing knee osteoarthritis.1 The incidence of ACL injuries is currently estimated at approximately 200,000 annually, with 100,000 ACL reconstructions performed each year.2,3
People who sustain ACL tears can choose between two options for treatment: structured rehabilitation and surgical reconstruction. In the US, surgical reconstruction is the more common choice, particularly in younger patients seeking to return to their normal level of physical activity and to sports that involve cutting and pivoting. Structured rehabilitation is used more commonly among less active and older patients. Although both treatments are considered cost-effective, few studies have assessed the short- and long-term economic effects on society of pursuing one treatment over the other.
In a study published in the Journal of Bone and Joint Surgery,4 we explored the cost-effectiveness of ACL reconstruction performed at 10 weeks or less after injury compared with rehabilitation. We estimated the societal and economic impact of ACL tears and surgical treatment for two time horizons: short-term outcomes (up to six years) and long-term outcomes (lifetime). Examination of the shorter-term outcomes contributes to understanding of which treatment options are appropriate for an unstable knee due to an ACL injury. The longer-term perspective accounts for the link between ACL injuries and osteoarthritis.
Analytic framework
We conducted cost-utility analyses of ACL surgical reconstruction (ACLR) and rehabilitation and compared short-term and long-term outcomes associated with each treatment path using a Markov model, which is often used by pharmaceutical and medical device companies to demonstrate the economic value of their products in terms of medical costs avoided, improved patient health and functionality, societal economic benefits, and increased longevity. Our approach uses a Markov model that considers the timing and probability of different patient outcomes associated with alternative treatments, and the costs and benefits associated with each outcome.
 In our model, the potential value of either treatment path comes from two major sources: (1) clinical outcomes and improved quality of life and (2) nonclinical (economic) outcomes, such as reduced disability and long-term medical costs (direct cost savings) and improved productivity (indirect cost savings). For the short-term perspective, we estimated indirect costs by examining the effects of functional limitations due to the ACL tear on work status, earnings, and disability payments. For the long-term analyses, it was assumed that some patients would develop osteoarthritis of the knee, which would sometimes progress to end-stage osteoarthritis.
In our model, the potential value of either treatment path comes from two major sources: (1) clinical outcomes and improved quality of life and (2) nonclinical (economic) outcomes, such as reduced disability and long-term medical costs (direct cost savings) and improved productivity (indirect cost savings). For the short-term perspective, we estimated indirect costs by examining the effects of functional limitations due to the ACL tear on work status, earnings, and disability payments. For the long-term analyses, it was assumed that some patients would develop osteoarthritis of the knee, which would sometimes progress to end-stage osteoarthritis.
Thus, we estimated indirect costs associated with knee osteoarthritis and total knee arthroplasty. One important aspect of our model is that we did not allow a patient in the rehabilitation treatment path to cross over to the ACL repair treatment path. We simulated the treatment path this way because our goal was to estimate the economic impact of access to ACL repair. In so doing, our model is assessing the value of having access to surgery to repair an ACL tear, but overstates the benefits of early ACL repair compared with rehabilitation and delayed ACL repair. We applied our model to a cohort representative of the population in the MOON (Multicenter Orthopaedic Outcomes Network) database.5
In a related study published recently in the American Journal of Sports Medicine,6 we performed an economic analysis of the KANON (knee anterior cruciate ligament non-surgical versus surgical treatment) trial, which did account for the crossover reported in that study. In addition, this study examined only direct costs. We found early ACL reconstruction was $1572 cheaper than structured rehabilitation and optional delayed reconstruction. The high crossover rate of 38% in the KANON trial and the not insignificant cost of rehabilitation drove these findings.
In these analyses, we estimate the ratio between the cost (direct and indirect) of the treatment (surgery or rehabilitation) and the benefits of the treatment, which are typically expressed in quality-adjusted life years (QALYs). The QALY is a measure of both length of life and quality of life in a single index number ranging from 0 to 1. One year of life lived in perfect health is worth 1 QALY (1 year of life × 1 utility value = 1 QALY), while a year of life lived in a state of less-than-perfect health is worth less than 1. The incremental cost-effectiveness ratio (ICER) is the ratio between the difference in costs and the difference in benefits of the two treatment options. That is, ICER = (CostReconst – CostRehab)/(QALYReconst – QALYRehab). Our outcome measures are mean costs and effectiveness (in QALYs) as well as ICER for each strategy.
Data sources
Patient-reported outcomes data for the short-term perspective came from the MOON database and the KANON study. Outcomes data for the long-term perspective came from the literature. The SF-6D was used to assess health utilities—measures of the strength of patients’ preferences for different health outcomes. Direct medical costs (rehabilitation, ACL reconstruction, knee arthroscopy, and revision procedures) were estimated, starting with the national mean Medicare reimbursements for the procedures in 2012 US dollars. We then extrapolated those costs using the payment rates of other insurers (as a percentage of the Medicare rate) and the national distribution of payers to estimate all-payer costs.
For the estimation of indirect costs, we used a two-step approach. First, we estimated the relationship between functional status and economic outcomes, utilizing data from the National Health Interview Survey (NHIS). The NHIS collects information from a stratified random sample of the US population regarding physical function, economic factors such as employment status and income, and other patient characteristics. For functional limitations, the NHIS asks respondents to rate how difficult it is for them to perform such tasks as walking a quarter mile or standing up for two hours.8 The second step was to use patient-reported outcomes involving functional status to estimate outcomes with and without surgery. The patient-reported outcomes included the KOOS (knee injury and osteoarthritis outcome score) and SF-36 from the MOON ACLR cohort. The questions in the NHIS matched questions in the KOOS and SF-36, which allowed us to populate the indirect cost model with data directly from MOON.
Findings
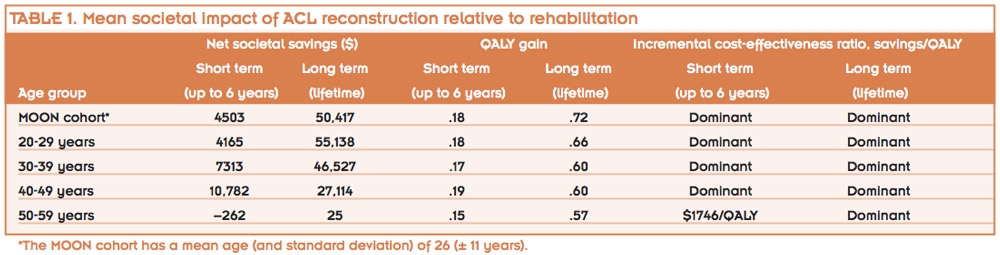
In the short term, ACL reconstruction was both less costly (a cost reduction of $4503) and more effective (a QALY gain of .18) compared with rehabilitation (see Table 1). In the long term, the mean lifetime cost to society for a typical patient undergoing ACL reconstruction was $38,121 compared with $88,538 for rehabilitation. Thus, in the long term, ACL reconstruction resulted in a mean incremental cost savings of $50,417 while providing an incremental QALY gain of .72 compared with rehabilitation.
The relatively young mean ages of the MOON and KANON cohorts, particularly MOON, represent the actual population experiencing ACL tears and undergoing ACL reconstruction. The average age of an ACL tear is quite young, typically occurring just at the beginning of or prior to the working part of a person’s lifetime, which is what drives the economic impact of ACL tears.
In cost-effectiveness analyses, a strategy is termed dominant when it is both less costly and more effective than an alternative. Therefore, ACL reconstruction was shown to be a dominant treatment strategy, and no incremental cost-effectiveness calculation was necessary for comparing the two strategies. A driving factor behind the higher effectiveness of ACL repair compared with rehabilitation is the higher probability of an unstable knee and associated lower utility in the rehabilitation group.5,7 That is, some patients who undergo rehabilitation only will have an unstable knee, which can result in additional injuries, such as meniscus tears or other significant injuries. In fact, our results were most sensitive to the rate of knee instability after initial rehabilitation: the higher the chance of having an unstable knee with rehabilitation alone, the greater the benefits of early ACL repair.
The lifetime burden of ACL tears in the US was estimated to be $7.6 billion annually (expressed as the net present value) when treated with ACL reconstruction and $17.7 billion annually when treated with rehabilitation. If all of these individuals were treated with ACL reconstruction, 118,000 patients would develop radiographic osteoarthritis over their lifetime, 31,600 of these would become symptomatic, and 25,800 would need a total knee arthroplasty. In comparison, if all were treated with the rehabilitation strategy, 140,000 patients would develop radiographic osteoarthritis, 38,000 of these would become symptomatic, and 30,800 would need a total knee arthroplasty.
As with all modeling approaches, the findings are sensitive to our assumptions.9 Because of uncertainty around some of the factors—such as the likelihood of an unstable knee after rehabilitation of an ACL tear—we modified our assumptions within reasonable ranges to assess the impact of the changes on our findings. These analyses demonstrated that ACL reconstruction was still the dominant treatment strategy. One important finding of these sensitivity analyses is that the cost of an ACL tear is low for most patients, but the high cost of an unstable knee in a fraction of the patients drives up the total economic burden substantially.
Conclusions
The analysis demonstrates that limiting access to ACL reconstruction may be harmful to patients and costly to society. In both the short and the long term, ACL reconstruction produced greater quality-of-life improvements at a lower cost compared with rehabilitation only. Patients who experience an ACL tear and suffer from an unstable knee afterwards experience not only losses in their quality of life, but also financial losses that impact not only them, but also their employers and society as a whole. These substantial indirect costs (lost wages, lower productivity, and higher disability payments) are largely associated with an unstable knee rather than with the development of knee osteoarthritis.
Both ACL reconstruction and rehabilitation treatment strategies are likely to yield high-quality, low-cost care when performed for the appropriate patient. In the short term, opportunities for improving treatment for ACL tears reside in better understanding patient preferences and in patient-centered care. For example, a patient who is at risk of low knee-related quality of life due to an unstable knee might be better treated with early ACL reconstruction, whereas a low-demand patient who has a lower-than-average risk of symptomatic instability could undergo rehabilitation as an initial treatment.
This study demonstrated the potential effects of minimizing meniscal injury on the rates of symptomatic osteoarthritis and total knee arthroplasty. However, research is needed to document progression from meniscal injury to radiographic osteoarthritis and to symptomatic osteoarthritis. As these are long-term outcomes, proxy measures for osteoarthritis (such as biomarkers) will be an important component of such future studies as well.
ACL reconstruction was shown to be cost saving and more effective in both the short term and the long term. Long-term outcomes, though less certain, appeared to increase only the cost savings of the ACL reconstruction strategy. Substantial downstream effects of ACL tears exist. These findings support greater attention on preventive injury strategies and early intervention to prevent osteoarthritis. Greater study involving patient-centered care is necessary to determine the optimal treatment strategy for individual patients and providers, but the present study demonstrated that access to ACL reconstruction is critical to optimal societal healthcare delivery.
Richard C. Mather III, MD, is assistant professor of orthopaedic surgery in the Division of Sports Medicine, Department of Orthopaedic Surgery, at Duke University Medical Center in Durham, NC. Lane Koenig, PhD, is founder and president of KNG Health Consulting, a health economics and health policy research firm based in the Washington, DC, area.
1. Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 2009;37(7):1434-1443.
2. Miyasaka KC, Daniel DM, Stone ML. The incidence of knee ligament injuries in the general population. Am J Knee Surg 1991;4:43-48.
3. Brown CH Jr, Carson EW. Revision anterior cruciate ligament surgery. Clin Sports Med 1999;18(1):109-171
4. Mather RC 3rd, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am 2002;95(19):1751-1759.
5. Unpublished data provided by the Multicenter Orthpaedic Outcomes Network (MOON), which was established in 2001 to examine how patients fare after undergoing an anterior cruciate ligament reconstruction. This NIH-funded consortium consists of 18 sports medicine physicians across seven sites and has enrolled more than 3500 patients who receive follow-up evaluations at two and six years postsurgery. https://medschool.vanderbilt.edu/orthopaedics/moonmars-project.
6. Mather RC 3rd, Hettrich CM, Dunn WR, et al. Cost-effectiveness analysis of early reconstruction versus rehabilitation and delayed reconstruction for anterior cruciate ligament tears. Am J Sports Med 2014 May 6. [Epub ahead of print]
7. Frobell RB, Roos EM, Roos HP, et al. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 2010;363(4):331-342.
8. National Health Interview Survey. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/nhis.htm. Last updated June 12, 2014. Accessed June 18, 2014.
9. Mather RC 3rd, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am 2002;95(19):1751-1759.