When conservative therapies fail, surgical reconstruction of the foot is often required to restore function, heal ulcerations, and decrease risk of amputation in patients with CN. External fixation remains a reliable method, with plenty of advantages.
When conservative therapies fail, surgical reconstruction of the foot is often required to restore function, heal ulcerations, and decrease risk of amputation in patients with CN. External fixation remains a reliable method, with plenty of advantages.
By P. Tanner Shaffer, DPM, Jonathan Hook, DPM, FACFAS, and Ben Potter, DPM
Within the past decade, the worldwide prevalence of diabetes has increased from 4% to 6.5%, prompting the World Health Organization to classify diabetes as a 21st century epidemic.1 Within the United States, more than 100 million adults are now living with diabetes or prediabetes, according the Centers for Disease Control.2 As of 2020, 34.2 million Americans—10.5% of the US population—have diabetes, while another 88 million have prediabetes, a condition that, if left untreated, often leads to type 2 diabetes within 5 years. Sadly, the rate of new diabetes diagnoses, which is linked to the rising rate of obesity, remains steady.
With the increase in prevalence, the total estimated economic cost of diabetes in the US has increased more than 25% to $327 billion, up from $245 billion over a span of only 5 years (2012-2017).3 Approximately 700,000 people were diagnosed with diabetes per year during that time and prevalence is expected to increase as the population grows and ages. As the population of patients with diabetes grows, medical professionals manage more diabetic complications on a day-to-day basis. One such complication is Charcot Neuroarthropathy (CN). While CN is also associated with a multitude of etiologies (eg, tertiary syphilis, alcoholic peripheral neuropathy, spinal cord injuries, renal dialysis), the majority of today’s cases are associated with severe peripheral neuropathy secondary to diabetes. Based on several population-based studies, the prevalence of CN is estimated to be 0.4 – 13%; however, CN is also associated with a high level of mistaken or delayed initial diagnosis—nearly 80% in one study.4 Presently, an estimated 150,000 US patients with diabetes suffer with CN.
Pathophysiology
Charcot Neuroarthropathy is a rapidly progressive hypertrophic osteoarthropathy that leads to severe foot and ankle deformities.4 CN weakens the ligaments and bones in structures that undergo substantial stress (particularly the foot), causing collapse, fracture, and joint destruction.5 Although the consequences of this limb-threatening complication have been known since it was first described in 1883, its etiology was elusive.6 Traditionally, two competing theories were used to describe its mechanism—the Neurotraumatic Theory and the Neurovascular Theory. The Neurotraumatic Theory states that CN is caused by unperceived trauma to an insensate foot. Sensory neuropathy then leaves the patient unaware of subsequent microtraumas that, over time, cause osseous breakdown. The Neurovascular Theory postulates that autonomic neuropathy of blood vessels leads to arteriovenous shunting of blood into bone. This, in turn, causes the bone to become ‘washed out’ of its minerals, leading to breakdown secondary to bony resorption.7 Today, it is accepted that CN is caused by a combination of both theories: Autonomic neuropathy with repeated microtrauma (typically from ambulation) leads to increased hyperemia/inflammation, increased osteoclastic activity (osteopenia), and bone/joint destruction and deformity.
While CN can affect any joint under substantial stress, it more often affects the weight-bearing bones and joints of the foot and ankle. The most common area of the foot involved is the midfoot.8 Brodksy, who classified CN based on its joint location in the foot and ankle, reported that approximately 60% of CN cases affected the tarsometatarsal joints or the naviculocuneiform joints.9 Osseous destruction of the midfoot leads to the classic ‘rocker-bottom’ deformity associated with midfoot CN. Rocker bottom deformity imparts a 4-fold increase in risk of ulceration in CN patients versus other diabetic feet.10
External Fixation
Peripheral Arterial Disease in Patients with Diabetic Charcot Neuroarthropathy
Peripheral arterial disease (PAD) has been a common finding in patients with diabetes, both types 1 and 2, for decades. However, its specific prevalence in patients with Charcot neuroarthropathy (CN) was not well defined until recently. In 2016, Wukich and colleagues designed a study to evaluate the prevalence of PAD in patients with CN, both with and without ulceration, compared to patients with diabetic foot ulceration (DFU) but no CN. Using lower extremity noninvasive arterial testing, they compared the test results of 85 patients with CN with the results of 126 patients with DFU but no CN. Although prevalence of PAD was 40% in the group with CN, it was less likely in the group with CN compared to the group with DFU (see graphic). Furthermore, patients with CN were 82% less likely compared to patients with DFU to have critical limb ischemia (CLI), defined as great toe pressure <30mm Hg.
Compared with patients with DFUs, the patients with CN were
- Less likely to have PAD: odds ratio [OR] 0.48 (95% confidence interval [CI] 0.28 to 0.85; P = .0111)
- Less likely to have ischemia: OR 0.33 (95% CI 0.16 to 0.69; P = .0033)
- Less likely to need for revascularization: OR 0.27 (95% confidence interval 0.10 to 0.73; P = .0097)
They concluded that: PAD in patients with CN is not uncommon; however, CLI and the need for revascularization were significantly less likely than in patients with DFU without CN.
Source: Wukich DK, Raspovic KM, Suder NC. Prevalence of peripheral arterial disease in patients with diabetic Charcot Neuroarthropathy. J Foot Ankle Surg. 2016;55(4):727 – 731.
The main goal in treating midfoot CN is to create a stable plantigrade foot, with no wounds or infection, that can be placed in a custom diabetic shoe or brace.11 Conservative measures are often attempted initially and are aimed at preventing deformity progression and offloading ulcerated or at-risk areas. Total Contact Casting (TCC) is widely considered the conservative ‘gold standard’ and is indicated for CN of the midfoot as well as forefoot. However, while effective at offloading, TCC and other conservative modalities do not correct refractory deformity after CN has progressed. In these cases, surgical reconstruction of the foot is often required to restore function, heal ulcerations, and decrease risk of amputation.11
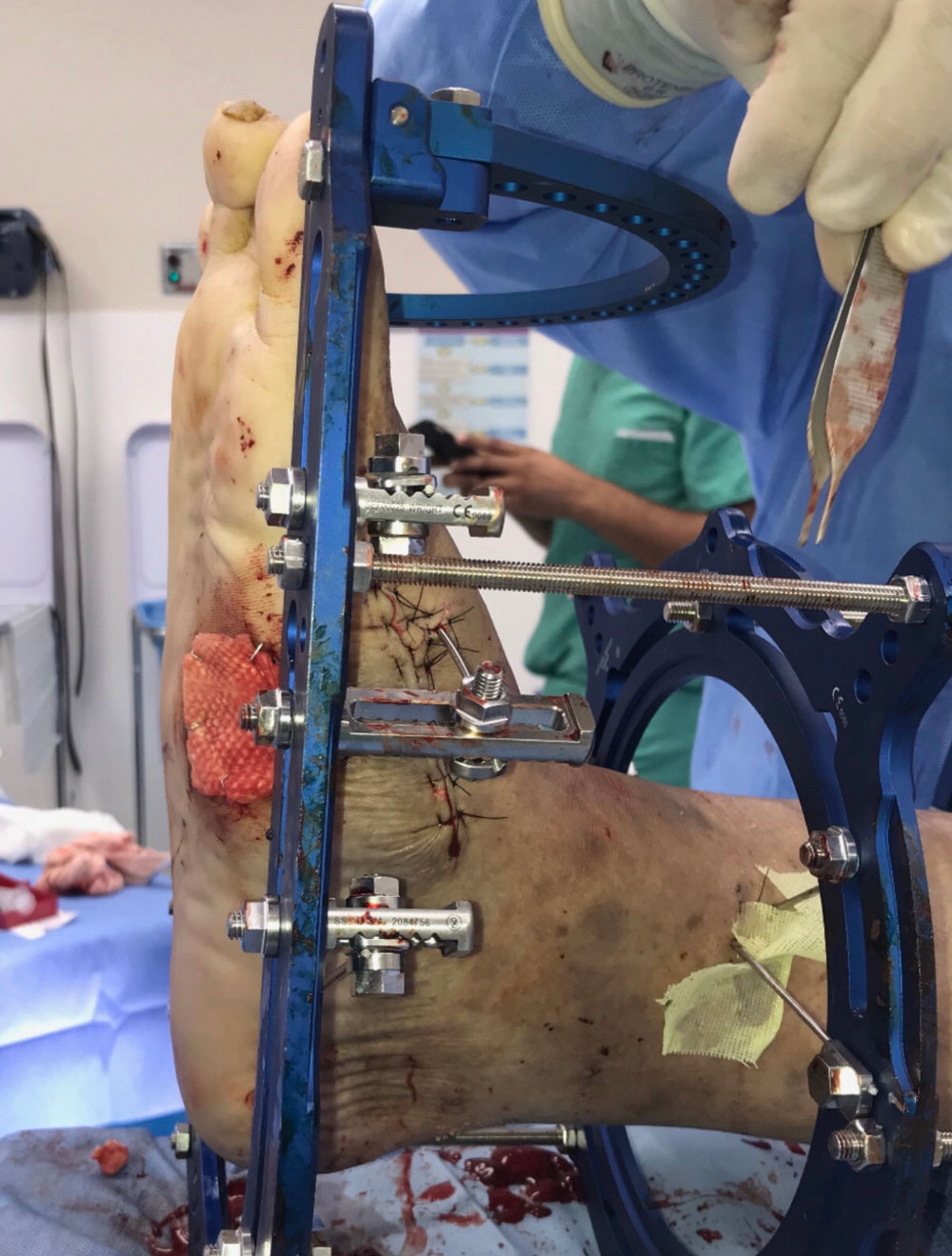
While many different surgical techniques are advocated for deformity correction for CN, external fixation remains a reliable method. This is due to several advantages. External fixation:
- Can Be Utilized in the Setting of Infection: Whereby internal fixation is contraindicated in the setting of acute osteomyelitis or cellulitis (due to bacterial seeding and biofilm formation), external fixation can span or bypass areas of infection.12 In fact, external fixation is often used as an alternative to maintain deformity correction when internal fixation is removed due to infection.
- Is Minimally Invasive: When compared to internal plates and intramedullary nails, external fixators cause less disruption of the soft tissue, osseous blood supply, and periosteum.13 This is particularly important in patients with poor healing potential such as those with osteoporosis, a poor soft tissue envelope, or peripheral vascular disease (though less common in CN patients; see Peripheral Arterial Disease in Patients With Diabetic Charcot Neuroarthropathy, page 27).
- Allows for Early Weight Bearing: External fixation allows for earlier ambulation when compared to other surgical constructs. This is an advantage because, in general, the patient population with diabetes tends to be non-compliant. A study in 2016 found that 27.5% of patients with diabetes were non-compliant with weight-bearing restrictions post-operatively. Of those patients, 50% went on to experience adverse events.14 Since many patients with CN will inevitably walk despite restrictions, a construct stout enough for them to ambulate earlier improves their outcomes.
- Allows for Both Immediate and Gradual Correction: While static external fixation can be used to stabilize osteotomies or fusion sites, dynamic external fixation allows for multiplanar deformity adjustment at the surgeon’s discretion.12 Immediate, single stage correction can occasionally cause neurovascular compromise and soft tissue necrosis from overstretching of structures. External fixation allows the provider to dial in and adjust correction over a longer period to avoid this.15
- Allows Simultaneous Soft Tissue Care/Wounds Can Be Addressed Simultaneously With External Fixation: External fixation allows the surgeon to easily assess and manage concomitant open wounds during postoperative care. In acute or chronic open wounds with CN, staged soft tissue reconstruction is frequently required in addition to osseous work to attain wound closure. External fixation can be used as an adjunct to allow soft tissue flaps to be offloaded/protected and closely monitored in the post-operative period.12,16
- Is an Extremely Strong Fixation Construct: In a cadaveric biomechanical study by Latt et al in 2015, external fixation was compared to compression screws for arthrodesis (joint fusion) across the midfoot.17 In measuring compression across midfoot joints (a requirement for midfoot fusion surgeries in CN), external fixation averaged 186% of the amount of compression achieved by screws alone. Furthermore, external fixation can be extended well beyond the primary surgical area, adding to its inherent stability.
- Can Be Utilized in the Acute Phase of CN: CN has several stages in its progression (first described by Eichenholz). In the acute stage (0-1) of CN, the foot is clinically red, hot, and swollen due to hyperemia of the soft tissue and underlying bony structures. Some consider this a relative contraindication to internal fixation because of a compromised soft tissue envelope (due to swelling) and poor bone purchase from osteopenia. However, because of its minimally invasive nature and lack of dependency on cortical purchase for stabilization, external fixation can successfully provide deformity correction in this setting.18
Although it is a reliable construct for fixation in patients with midfoot CN, external fixation is not without its drawbacks. It is bulky, can be expensive and time consuming, and requires regular follow up. In a retrospective review of a level 1 trauma center, Chaus et al reported an average cost per external fixation frame of $5900.19 This cost analysis highlights the importance of using external fixation for CN only when necessary.
Furthermore, pin tract infections occur quite frequently, with up to 100% occurrence rate; however, most studies report a rate of approximately 20%.5 Significantly, nearly all such infections can be managed through local pin care alone or with oral antibiotics. Parameswaren et al published a retrospective review of 285 patients who underwent external fixation; only 3.1% developed pin tract infections that actually necessitated pin removal.20
 A Word About Outcomes
A Word About Outcomes
There is a paucity of strong evidence for outcomes regarding different methods of surgical fixation for CN reconstruction; however, a systematic review by Dayton et al in 2015 provides some substantial findings.21 It compared outcomes and complications between internal and external fixation constructs used to treat CN of the ankle as well as the foot. A total of 23 studies were included: 12 studies with 275 cases where internal fixation was used and 11 studies with 341 cases where external fixation was used. Overall, internal fixation carried an odds ratio for a successful outcome of only half that of external fixation (odds ratio 0.52; P < 0.05). When taking a closer look at only midfoot CN, there was no significant difference between success rates for internal versus external fixation. However, the study data revealed that external fixation was utilized more often in complicated cases involving osteomyelitis or large wounds—cases where internal fixation clearly would have had little success.
In summary
Charcot Neuroarthropathy is a debilitating complication of diabetes that affects approximately 150,000 US patients with diabetes. Deformity associated with CN imparts a significantly increased risk of ulceration and amputation in this medically complex population, and healthcare providers are being encouraged to manage associated complications more aggressively, which translates to more frequently. In doing so, external fixation is being utilized more and more to address CN deformities. Research shows that it is an incredibly versatile construct that can treat all forms and stages of CN with a high level of success. Though sometimes costly and time consuming, its utility in complicated cases with complex deformities cannot be denied.
Tanner Shaffer, DPM, is a Resident Foot and Ankle Surgeon at Mercy Hospital & Medical Center in Chicago, Illinois.
Jonathan Hook, DPM, FACFAS, is affiliated with the podiatric residency program at Mercy Hospital and Medical Center in Chicago, Illinois. He is in podiatric practice, specializing in foot, rearfoot reconstruction, and ankle surgery at Midland Orthopedic Associates in Chicago.
Ben Potter, DPM, is a Resident Foot and Ankle Surgeon at Mercy Hospital & Medical Center in Chicago, Illinois.
- Rios-Ruh JM, Martin-Oliva X, Santamaría-Fumas A, et al. Treatment algorithm for Charcot foot and surgical technique with circular external fixation. Acta Orto Mex. 2018;32(1):7-12.
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020.
- American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care. 2018 Mar; dci180007. Available at https://doi.org/10.2337/dci18-0007. Accessed May 20, 2020.
- Milne TE, Rogers JR, Kinnear EM, et al. Developing an evidence-based clinical pathway for the assessment, diagnosis and management of acute Charcot Neuro-Arthropathy: a systematic review. J Foot Ankle Res. 2013;6:30.
- Dodd A, Daniels TR. Charcot Neuroarthropathy of the foot and ankle. J Bone Joint Surg (Amer Vol). 2018;100(8):696-711.
- Rogers LC, Frykberg RG, Armstrong DG, et al. The Charcot foot in diabetes. Diabetes Care. 2011;34(9):2123-2129.
- Varma AK. Charcot neuroarthropathy of the foot and ankle: a review. J Foot Ankle Surg. 2013;52(6):740-749.
- Salini D, Harish K, Minnie P, et al. Prevalence of Charcot arthropathy in type 2 diabetes patients aged over 50 years with severe peripheral neuropathy: a retrospective study in a tertiary care south Indian Hospital. Indian J Endocrinol Metab. 2018;22(1):107-111.
- Brodsky JW. The Diabetic Foot. In: Coughlin MJ, Mann RA, Saltzman CL, editors. Surgery of the Foot and Ankle. 8th ed. St. Louis, MO: Mosby;2008. Pp. 278-283
- Larsen K, Fabrin J, Holstein PE. Incidence and management of ulcers in diabetic Charcot feet. J Wound Care. 2001;10(8):323.
- LaPorta GA, D’Andelet A. Lengthen, alignment, and beam technique for midfoot Charcot Neuroarthropathy. Clin Podiatr Med Surg. 2018;35(4):497-507.
- Shibuya N. The Charcot Foot. In Lee MS, Grossman, eds. Complications in Foot and Ankle Surgery Management Strategies. Springer International Publishing: 2017;329.
- Fragomen A, Rozbruch S. The mechanics of external fixation. HSS Journal. 2007;3(1):13.
- Manway JM, Blazek CD, Burns PR. Special considerations in the management of diabetic ankle fractures. Curr Rev Musculoskelet Med. 2018;11(3):445-455.
- Ramanujam CL, Zgonis T. An overview of internal and external fixation methods for the diabetic Charcot foot and ankle. Clin Podiatr Med Surg. 2017;34(1):25-31.
- Short DJ, Zgonis T. Circular external fixation as a primary or adjunctive therapy for the podoplastic approach of the diabetic Charcot foot. Clin Podiatr Med. Surg. 2017;34(1):93–98.
- Latt LD, Glisson RR, Adams SB, Schuh R, Narron JA, Easley ME. Biomechanical comparison of external fixation and compression screws for transverse tarsal joint arthrodesis. Foot Ankle Int. 2015;36(10):1235.
- Schade VL, Andersen CA. A literature-based guide to the conservative and surgical management of the acute Charcot foot and ankle. Diabet Foot Ankle. 2015; 6:26627.
- Chaus GW, Dukes C, Hak DJ, Mauffrey C, Mark Hammerberg E. Analysis of usage and associated cost of external fixators at an urban level 1 trauma centre. Injury. 2014;45(10):1611-1613.
- Parameswaran AD, Roberts CS, Seligson D, et al. Pin tract infection with contemporary external fixation: how much of a problem? J Orthop Trauma. 2003;17(7):503-507.
- Dayton P, Feilmeier M, Thompson M, Whitehouse P, Reimer RA. Comparison of complications for internal and external fixation for Charcot reconstruction: a systematic review. J Foot Ankle Surg. 2015;54(6):1072-1075.