This two-part series examines trends and techniques in materials development and fabrication. This second installation focuses on technological advances that are likely to affect the structural properties and manufacture of in-shoe foot orthoses.
This two-part series examines trends and techniques in materials development and fabrication. This second installation focuses on technological advances that are likely to affect the structural properties and manufacture of in-shoe foot orthoses.
By Cary Groner
Advances in plastics and materials science have significantly advanced the design and manufacture of foot orthoses over the past couple of decades, but new compounds and fabrication methods have the potential to transform the field, according to experts. Novel composites and hybrid plastics will offer lighter, stronger, and more customizable devices, and the way these orthoses are built means some materials popular today will become obsolete, replaced by others invented specifically for use with new manufacturing techniques.
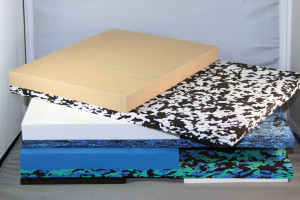
Practitioners and fabricators already have a dizzying array of materials at their disposal, including thermoplastic polyolefins (polypropylene, polyethylene, and copolymer combinations of them); polyethylene foams (e.g., Plastazote, Nickelplast); open-cell polyurethane foam (Poron); ethylene vinyl acetate (EVA); closed-cell neoprene foam (Spenco); thermoset carbon-fiber composites; new compounds that put layers of carbon fiber between polyolefins (e.g., continuous-fiber thermoplastic); and others, such as natural and artificial cork.1
Which of these a practitioner uses, and in what combinations, depends on individual preference and on the needs of the patient.
“It’s critical to understand how these different materials work,” said Kevin Kirby, DPM, an adjunct associate professor at the California School of Podiatric Medicine at Samuel Merritt College in Oakland. “Some resist compression but have very little torsional stiffness; that class is called shank-dependent and includes the various foam products. Shank-independent materials, by contrast, have their own internal rigidity, so they can act independently of the shoe shank to resist deformation from the foot.” That category, Kirby explained, includes thermoplastics and carbon composites.
The two shank tribes associate closely with each other, of course. The independents need the dependents, as it were, because polypropylene and composite orthoses usually require something softer on top for comfort. Shank-dependent materials, how- ever, are typically used alone, and are in full contact with the bottom of the shoe, unlike harder materials.
“Softer materials like EVA, Poron, and polyurethane rely on sitting on the shoe bed, whereas carbon fiber and thermoplastics will generally contact the shoe only under the heel segment and at the distal end,” explained Simon Spooner, PhD, a podiatrist in Plymouth, England.
Durometer vs density
One striking characteristic of modern foam products is the extraordinary compression resistance (durometer) that can be achieved with so little weight. Durometer and density are different, however, and gains in lightness can mean losses in durability.
For example, Susan Rawles, CPed, orthotics production manager at Shu-Re-Nu in Atlanta, told LER she’s in the process of switching from Chinese to German EVA due to density issues.
“Density is more important than durometer,” Rawles said. “Chinese EVA has a lot more air blown into it than German EVA, and, when I mill both products, I can feel the difference in density even though the durometer is the same.”
German EVA also handles a lot more compression, according to Rawles.
“If you put a 120-pound woman on the Chinese EVA, it may last two or three years, but if you put on a 250-pound man, it’s bottoming out,” she said.
She added that consistency is a problem with Chinese foam.
“One day the Chinese factory is making pool toys, and the next day it’s making orthotic blanks,” she noted. “The German company is making EVA strictly for the orthotics market, so the quality is consistently excellent from batch to batch.”
Rawles has noticed differences in blank manufacturing, as well. Dual-durometer Chinese orthosis blanks have a tendency to separate where the 55-durometer heel section meets the 45-durometer forefoot section, she said. The vulcanized German products don’t have that problem.
“I never want to tell a customer that the product won’t come apart unless I’ve tested it myself,” she said. “The German [dual-density] blanks—I’ve heated them, I’ve tried everything, but you’re not getting that stuff apart. It’s amazing material.”
That the German sheet EVA is available in a 35-mm thickness helps, too.
“If I have someone with a very pes cavus foot, or who needs a deep heel cup, I can use the thirty-five millimeter to achieve a higher arch or a deeper cup,” Rawles said. “That extra five millimeters [over the standard 30-mm thickness] makes a huge difference.”
Surprisingly, by moving from Chinese blanks to German sheet stock that will be cut with a router, Rawles is saving money, too.
“I’ll be reducing my costs from about twenty-eight dollars a pair to about fifteen dollars a pair,” she said.
According to industry sources, the ratio of ethylene to vinyl acetate in EVA is adjusted to affect durometer. Orthopedic EVA generally contains 14% to 28% vinyl acetate, and higher amounts of ethylene increase the material’s plastic characteristics or hardness. Because these active ingredients typically constitute less than half of the ingredients in EVA, however, decisions about fillers and additives are also important, as they too can affect the final product’s density and texture.
Geometry 101
Experts stress that the material itself isn’t the only determinant of how stiff or how giving an orthosis is in practical application, however; surface geometry is crucially important as well.
“Foot orthoses work by modifying the reaction forces at the foot–orthosis interface,” Spooner said. “They can do that in only three ways—by modifying the surface topography of that interface, by modifying its load deformation characteristics, or by modifying its friction characteristics.”
Spooner refers to durometer measurement as a “blunt instrument,” noting that it applies mainly to the flat sheet material used in the orthosis. He prefers to assess devices by their stiffness, which he defines as load divided by deformation.
“Surface geometry will define stiffness, and that stiffness varies from point to point on the orthosis,” he said. “That will ultimately define the reaction forces that occur between the foot and the orthosis. Load deformation is very important—but deformation of the finished orthosis, not the material per se.”
Orthoses with high deformation characteristics arrest force and reach equilibrium more rapidly than those with lower deformation characteristics, Spooner continued.
“Stiffer material applies higher reaction forces—braking forces, if you will—than more compliant materials,” he said. “In some circumstances that might be beneficial; in others it might not. The real trick is manipulating the surface geometry and the load deformation characteristics of the final orthosis so that we have areas with high reaction forces and areas with lower reaction forces. We’re actually shifting the center of pressure to achieve the kinetic response we desire and offload tissue that is in pain.”
Friction is an important consideration as well, particularly in diabetic patients who may be more susceptible to foot ulcers.
“Friction in orthoses usually occurs in the interface between the top cover and the wearer’s hosiery material,” Spooner said. “You want the top cover to have a lower coefficient of friction in its interface with the hosiery than that between the hosiery and the skin, or the shear will occur at the latter and could lead to ulceration.”
Because of the ulcer risk associated with diabetes, insole materials have been closely studied in those populations—though not surprisingly, conclusions often differ.
For example, an early study from 1995, conducted at the Mayo Clinic, compared three compounds commonly used to make shoe inserts for diabetic patients and found that polymeric foam rubber best attenuated impact force.2 A later paper reported that medium durometer Poron (22, 27, and 32 Shore) reduced mean walking pressures more effectively than both softer and firmer Poron (14, 17, and 55 Shore) when used as a flat sheet cut into the shape of an orthosis; however, the patients’ custom orthoses (composition not specified) reduced pressure best of all (55% vs 36%-39% for medium-durometer Poron).3
A 2007 study published in Foot & Ankle evaluated six materials in five clinically popular combinations and determined that two combinations—medium Plastazote plus Nickelplast and Nickelplast plus Poron—were the toughest. There was no difference in peak pressures between pretesting and post-testing after 100,000 stress cycles, whereas other combinations showed increased peak pressures after testing.4 Another paper from that year, also in Foot & Ankle, studied 15 commonly used foam materials and reported that two forms of 6-mm Poron (numbers 96 and 4000) were best for dampening impact, while high-density EVA was best for motion control.5
Decisions, decisions…
Not surprisingly, practitioners can feel a little overwhelmed by the sheer number of choices suggested by such data. Ultimately, the decision about a given patient’s needs depends on a variety of factors, including experience and personal preference. For Spooner, two critical factors are the patient’s weight and activity level.
“I work with professional rugby players who weigh about twenty stone [280 lbs] and can sprint nearly as fast as Usain Bolt,” he said. “Trying to provide foot orthoses that can cope with those kinds of forces is a challenge. You’ve got to pick the right horse for the right course.”
As noted earlier, Spooner believes that, from a biomechanical perspective, shape is at least as important as material. Research bolsters this position regarding comfort, as well. In a study published last year, Australian scientists reported that healthy individuals prioritized contouring over hardness when judging orthoses’ comfort.6
For Bruce Williams, DPM, owner of Breakthrough Podiatry in Merrillville, IN, decisions about materials begin with careful casting of the foot.
“How you cast a high-arched foot can make a huge difference in the flexibility or rigidity of the device,” he said. “For most patients, I dorsiflex the toes and try to cast the foot so that we maximize the lateral and medial midfoot arches.” He then typically uses either polypropylene or EVA for the orthosis.
Williams echoed Spooner’s view of the importance of geometry.
“Because of that arched structure, you can use a lower-density more flexible material and still come out with a very rigid device,” he said. “Even the EVA I use will sometimes be too rigid and require some grinding to gain more flexibility.”
Williams also appreciates that EVA is relatively forgiving in the fabrication process.
“If you take something off a polypropylene device, you can’t put it back,” he said. “In some cases, I use EVA because I can do a lot of forefoot and digital postings either built-in or as add-ons. Then, if you’re grinding and you take off too much, you can hot-glue EVA back on.”
Polypropylene, on the other hand, may be better when the patient is going to wear a device with multiple shoe types.
“It maintains rigidity within the structure [of the shoe], so you can put it right over a built-in arch, whereas if EVA doesn’t match the last, we may have to grind material away to accommodate it,” Williams said.
Williams also noted that polypropylene devices, because of their shank-independence, provide better stability than EVA when worn in softer and more flexible shoes.
Michael Gross, PT, PhD, a professor of physical therapy at the University of North Carolina at Chapel Hill, emphasized that decisions about materials and design are closely linked.
“When people decide to make an orthosis out of hard plastic, they have already made a second decision, which is that the orthosis has to end posterior to the metatarsal heads,” Gross said. “That means there can’t be effective posting in the forefoot.”
This limitation can prevent proper treatment, in his experience.
“When folks are pronating excessively, some practitioners pick a rigid material to control the excessive motion,” he said. “But in many cases, what’s driving that pronation is excessive forefoot varus, so I want to give them a medial forefoot post to address the problem directly. If they get a rigid orthotic instead, a lot of times they’ll complain of discomfort, because without the forefoot post their feet will be crashing into the orthotic’s arch.”
In such cases, Gross prefers to use a thin thermoplastic blank, molded to the patient’s foot contour, bolstered with softer materials such as thermal cork, and topped with either suede or EVA. He makes posts out of Nickelplast. When patients have metatarsalgia, he may grind away some of the Nickelplast and replace it with Poron.
Patients with diabetes require special consideration, he noted.
“Often they are given orthoses that are too soft, and as a result, the pressure applied to the bony prominences, which are the areas of greatest risk for pressure sores, is greater,” he said. “I prefer to build something with thermoplastic, then use cork to get a firm push into the fleshy arch, which is at low risk for ulceration. That way, I decrease pressures over the heel and metatarsal heads. I may then use a soft Plastazote to provide extra cushioning in the top cover.”
Fabrication
Other experts agree that materials and fabrication are increasingly linked in practical application.
“I don’t like working with carbon fiber, because the particulate you’re grinding off isn’t nice, even if you’re wearing a respirator,”said Simon Spooner. “I’ve also had more breakages with it. I’ve never had a polypropylene orthotic fracture, but if you get a little grit in your shoe, the [thermoset] resin scratches, the carbon cracks, and the cracks propagate. Also, the devices are so thin—about a millimeter, versus four to six millimeters for polypropylene—that I’ve seen them act like a knife and cut the upper away from the sole of the shoe.”
According to some experts, the new carbon-fiber reinforced thermoplastics improve on thermoset composites by providing a moldable and more crack-resistant outer layer.
Spooner considers 3D printing one of the most promising developments in orthosis fabrication.
“It’s a challenge to manipulate reaction forces, and now we’re doing it naively,” he said. “We could do it better by manipulating the load deformation characteristics of the orthosis itself by using materials of different densities, or by changing their thickness. With three-D printing, we can start having hollow sections within a shell, which create shapes in them like springs, so it doesn’t have to be a shell with a block in the back. We could have ‘smart shells’ designed using finite element analysis to pull the force one way or another.”
Spooner, with characteristic energy, is working on a variety of other promising technologies. One, selective laser sintering, would shoot lasers, placed at 90° to one another, through a liquefied or powdered plastic compound; where the beams cross, the material fuses into hard plastic. The approach, which, like 3D printing, falls under the rubric of “additive manufacturing,” could help realize the potential of CAD-CAM design, creating cavities and multiple shell thicknesses in the devices.
The approach has been tested successfully. In a study e-published last year, researchers at Loughborough University in the UK scanned the feet of 38 runners in 3D, then used laser sintering to produce custom insoles that had better comfort and fit than noncustom insoles.7
“Our goal was to see to what extent we could develop personalized sports footwear using additive manufacturing,” said Andre Salles, PhD, who conducted the study as part of his doctoral dissertation at the university. (Salles is now a research trainee at Adidas in Herzogenaurach, Germany.)
“The concept was to have something that would be quick and easy to implement in a shop,” Salles continued. “We wanted the customer to be able to have the foot scanned, then have the insoles manufactured right there.”
The researchers produced the custom insoles out of a polyamide material called nylon 12, then padded them by gluing on Poron.
“It’s feasible to use additive manufacturing to deliver orthotics,” Salles said. “Eventually we’d like to see if we could deliver the entire footwear, but that would be much more complicated.”
Non-Newtonian polymers, currently used by at least one running shoe company, also have potential for advancing the orthotics field, according to Spooner.
“These polymers change their characteristics depending on the rate of loading,” he said. “If you apply force slowly, they act like a liquid, but if you apply it quickly, they act like a solid. We could have ‘smart orthoses’ that are stiffer if you hit the ground hard, and softer if you’re standing there working on a machine.”
Spooner is also interested in replacing current plastics with greener materials such as polylactic acids, which are derived from plant starch, could be recycled or turned into fertilizer, and ideally could be used with 3D printers.
Changing relationships
New fabrication methods may change the relationship between practitioners and orthotic laboratories, Spooner added.
“Now, you send them a cast or a scan, then they make a device. In the not-too-distant future, they’ll create a digital orthosis and send it back to you, and you’ll have a 3D printer to make the device in your office,” Spooner said.
Some practitioners are already milling orthoses in-house using existing technology; only the machine would change with 3D printing. Moreover, practitioners wouldn’t be locked into that model if they didn’t want it; they could make orthoses on site or have a service bureau available, which would allow the centralization of both manufacturing expertise and capital expenditure.
Regardless of advances in materials, experts agree that it’s the people using them who’ll make the biggest difference.
“Ultimately, it’s not the materials, it’s the knowledge,” said Kevin Kirby. “The bottom line is: know your materials and know their limits, their strengths and weaknesses. You have to know how to use any material in the right geometry, with the right stiffness and the right shoe, to optimize the effect for your patient.”
Cary Groner is a freelance writer in the San Francisco Bay Area.
1. Foto JG, Birke JA. Evaluation of multi-density orthotic materials used in footwear for patients with diabetes. Foot Ankle Int 1998;19(12):836-841.
2. Shiba N, Kitaoka HB, Cahalan TD, Chao EY. Shock-absorbing effect of shoe insert materials commonly used in management of lower extremity disorders. Clin Orthop Relat Res 1995;(310):130-136.
3. Birke JA, Foto JG, Pfeifer LA. Effect of orthosis material hardness on walking pressure and high-risk diabetes patients. J Prosthet Orthot 1999;11(2):43-46.
4. Brodsky JW, Pollo FE, Cheleuitte D, Baum BS. Physical properties, durability, and energy-dissipation function of dual-density orthotic materials used in insoles for diabetic patients. Foot Ankle Int 2007;28(8):880-889.
5. Paton J, Jones RB, Stenhouse E, Bruce G. The physical characteristics of materials used in the manufacture of orthoses for patients with diabetes. Foot Ankle Int 2007;28(10):1057-1063.
6. Mills K, Blanch P, Vicenzino B. Influence of contouring and hardness of foot orthoses on ratings of perceived comfort. Med Sci Sports Exerc 2011;43(8):1507-1512.
7. Salles AS, Gyi DE. An evaluation of personalised insoles developed using additive manufacturing. J Sports Sci 2012 Oct 22. [Epub ahead of print]