Kinematic and kinetic alterations in the lower extremities that researchers have observed during the course of a prolonged run may provide clinically relevant insights into patellofemoral pain and other conditions associated with a gradual onset of symptoms during exercise.
Kinematic and kinetic alterations in the lower extremities that researchers have observed during the course of a prolonged run may provide clinically relevant insights into patellofemoral pain and other conditions associated with a gradual onset of symptoms during exercise.
By Lauren Benson, MS; and Kristian O’Connor, PhD
Many people choose running as a convenient and inexpensive type of physical activity. Running has increased in popularity since the 1970s,1,2 and not surprisingly the number of people injured while running has also increased. The percentage of runners who experience running-related injuries can be as high as 79.3% for lower extremity injuries.3 The most common site of injury is the knee, which accounts for up to 50% of running injuries,2-5 while patellofemoral pain (PFP) has consistently been the most common overuse running injury.2,4,6,7
Running injuries are typically the result of overuse or pain resulting from repetitive tissue (bone, cartilage, tendon, ligament, or muscle) microtrauma. These repetitive stresses are necessary for positive remodeling of tissue, and will not result in injury as long as the stresses are kept below critical limits. However, without sufficient time between applications of stress, repeated exposure of tissue to low-magnitude forces creates microscopic injuries that eventually strain the tissue until an overuse injury occurs.5,8-10
Impact forces, which result from contact between the foot and ground, contribute to these stresses in combination with lower extremity mechanics. Runners can manipulate hip and knee flexion, ankle dorsiflexion, and pronation at the subtalar joint to better absorb impact forces.11,12 However, poor mechanics while running can play a role in developing an overuse injury. For example, research suggests PFP is caused by excessive patellofemoral joint stress.13 Mean patellofemoral joint contact forces during running can be up to 7.6 times body weight; with many repetitions, this may explain why the patellofemoral joint is commonly injured.14,15 Frontal plane loading, characterized by an increased internal knee abduction moment throughout stance, has been associated with PFP in both retrospective and prospective studies.16 Excessive knee valgus movement has been shown to contribute to knee injuries, including PFP.17 Additionally, transverse and frontal plane rotations of the hip and knee can change the Q-angle; an increased Q-angle causes greater retropatellar stress during knee flexion. Performing weight-bearing activities, such as running, with this alignment may cause inflammation of the tissues around the patella and lead to PFP.15,18
Focusing on fatigue
 Since overuse injuries are considered the result of exposure to repetitive stresses, researchers often assess running mechanics during the course of a single running bout. Typically, the goal is to fatigue a runner and examine changes in lower extremity mechanics. However, there are several challenges when studying fatigue, including how it is defined and measured.
Since overuse injuries are considered the result of exposure to repetitive stresses, researchers often assess running mechanics during the course of a single running bout. Typically, the goal is to fatigue a runner and examine changes in lower extremity mechanics. However, there are several challenges when studying fatigue, including how it is defined and measured.
In relatively simple terms, fatigue can be considered a decrease in force production, such that there is an increase in the perception of effort required and, eventually, an inability to produce the force.19 This type of definition suggests fatigue occurs suddenly at task failure; however, the force-generating capacity begins to decrease at the onset of exercise. Therefore, fatigue may be more aptly defined as an exercise-induced reduction in maximal voluntary muscle force due to peripheral changes in the muscle and reduced drive from the central nervous system.20 It is possible that there is not one all-encompassing model of fatigue. The process by which a muscle becomes fatigued may have both central and peripheral factors, and is thought to be task-dependent.19-21
Fatigue in the context of exercise physiology has been objectively measured in terms of physiological effects, but it also has a subjective psychological component. Another term related to a reduction in performance during physical exercise is exhaustion. Exhaustion can be defined as the moment in which the sense of effort required to maintain a desired force is greater than a person’s willpower to maintain that output.22 Physiologically, fatigue due to running can be measured using blood lactate tests or a rating of perceived exertion. Heart rate can be used as a measure of effort.23 Fatigue, defined as a loss of force production, can be quantified in specific skeletal muscles by observing a decrease in force produced during a maximum voluntary contraction following a fatigue protocol. It can also be observed as a decrease in speed during a maximal-effort run.24
Task-dependent fatigue is related only to the characteristics of the exercise or task inducing the fatigue. Some studies use an exercise protocol designed to bring runners to the point of exhaustion or maximum fatigue. This could allow investigators to examine the greatest changes in biomechanics that occur as a result of exertion. However, many different exhaustion or maximum fatigue protocols have been used, and not all studies use objective, physiologically measured criteria for fatigue or exhaustion. Different running durations and intensities may affect runners differently.25 The shorter methods exhaust runners faster, yet may fatigue their cardiovascular system before compromising the neuromuscular system. The physiological and kinematic responses to this type of protocol have been reported to be different than responses to a longer protocol, such as a marathon run.25 Additionally, while training, runners rarely run to the point of exhaustion or maximum fatigue. Therefore, designing a study with a protocol that resembles a typical running session may give a more accurate picture of the biomechanical changes that occur during running.
Effects of prolonged running
Running in an exerted state occurs when runners perform a prolonged run at training pace until their heart rate reaches 85% of their maximum heart rate or they score higher than 17 (very hard) on a rating of perceived exertion scale.26,27 This protocol for running in an exerted state adopted by our lab closely mimics a typical bout of exercise for a runner, while also providing an objective measure of exertion for all participants.28,29
Runners with the most common running injury, PFP, often do not have pain at the beginning of a run, but complain of a gradual onset of pain as the run progresses.27 This may indicate that prolonged running or exertion could cause changes in mechanics that contribute to PFP. However, there have been very few studies investigating the effects of exertion on running mechanics in healthy and injured runners. Comparisons among the studies that have been completed in this field are difficult due to differences in exercise protocols, which have included a marathon run,30 a treadmill run at typical running speed,26 a shorter run at maximal effort,31 running until exhaustion at the ventilatory threshold,25 and other variations. Many studies that examine running in a natural environment utilize 2D data collection and report only changes in sagittal plane mechanics,30 though running injury is often related to frontal and transverse plane mechanics. Despite the discrepancies, there is some evidence in the literature and from a recent study in our lab29 suggesting that running in an exerted state may elicit mechanics that could contribute to running injury risk.
The goal of kinematic adaptations while running may be to minimize metabolic cost, even at the expense of shock absorption.32 However, shock attenuation, or the absorption of impact forces, is vital for the prevention of overuse running injuries. It can be accomplished due to the shock-absorbing properties of passive anatomical structures such as bone and the calcaneal fat pad, as well as external influences such as running shoes and the ground.33,34 Additionally, contraction of muscle plays a role in shock attenuation. It has been shown that muscle action at the joints, such as ankle eversion and ankle, knee, and hip flexion, help to reduce impact forces during running.34 Running in an exerted state may increase a runner’s risk of overuse injury if the muscle loses some shock-absorbing ability or causes a change in movement pattern.35
Exertion and running mechanics
Knee flexion at heel strike has been commonly studied after an exhausting run due to its role in shock attenuation. A few studies have reported no significant differences between pre- and postexercise knee flexion angle at heel strike,36-38 while others have reported an increase with fatigue in knee flexion angle at heel strike after a run.31,39,40 And, despite some evidence of an effect on sagittal plane knee angle at heel strike, this has not been seen throughout stance. Peak knee flexion angle during stance has been reported to decrease30 and increase,31 while some studies, including our recent publication, have reported no significant change.25-27,29 These equivocal results suggest a typical training run results in limited changes in knee flexion.
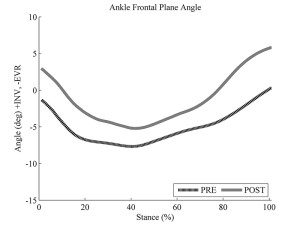
While rearfoot eversion plays a role in providing shock absorption during running, excessive rearfoot eversion, coupled with compensatory internal rotation of the tibia, knee, and hip, could put runners at risk for overuse injury.41 Previous work has shown an increase in maximum rearfoot eversion during stance, as well as an increase in maximum rearfoot velocity following a run in an exerted state.26,27,31,42 We also found a greater rate of rearfoot eversion in healthy female runners after running in an exerted state (Figure 1).29 Consistent with the theory that rearfoot eversion is linked to proximal transverse plane mechanics, this coincided with a greater rate of tibial internal rotation moment (Figure 2).29 Our results are in line with those reported by Dierks et al, who used a similar exercise protocol in their studies.26,27
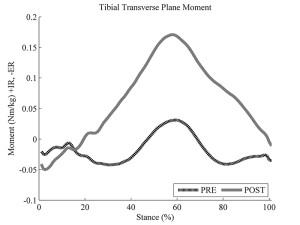
Figure 2. IR = internal rotation, ER = external rotation. Reprinted with permission from reference 29.
In addition to the changes at the ankle, we found changes in the transverse plane mechanics of the knee and hip. There was greater knee internal rotation (Figure 3) and a concurrent increase in hip internal rotation and decrease in hip internal rotation moment (Figure 4). The results of our study were generated using a waveform analysis that examines the mechanical effect over the entire duration of stance phase;29 results can be compared with the discrete analysis by Dierks et al that showed increases in knee internal rotation excursion, peak angle, and peak velocity,26,27 as well as an increase in hip internal rotation excursion.27
In general, the observed changes in rearfoot eversion and transverse plane mechanics at the ankle, knee, and hip suggest that runners may be in a more risky posture at the end of their typical training run than at the beginning.
Other effects of a run in an exerted state have been identified with regard to knee frontal plane mechanics. Focusing only on kinematic changes, Dierks et al showed that runners had decreased maximum knee adduction during stance, but a greater knee adduction excursion at the beginning of a typical training run compared with its completion.27 In contrast, our results showed a greater knee adduction angle throughout stance phase and a decrease in knee abduction moment when running in an exerted state (Figure 5).29 The frontal plane knee mechanics we observed may indicate that the healthy individuals in our study adopted this posture as a protection against potential knee pain.
Implications for injury
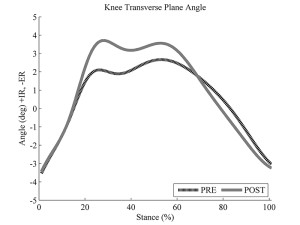
Figure 3. IR = internal rotation, ER = external rotation. Reprinted with permission from reference 29.
Examining the effects of a typical training run on mechanics for injured runners can provide insight about the mechanics of an injured state. Dierks et al showed that a group of runners with PFP had, in general, lower peak angles and maximum velocities than a control group, even for variables thought to cause or exacerbate PFP, including rearfoot eversion, components of knee valgus, and internal rotation of the tibia, knee, and hip.27 It is possible that these kinematics, which are opposite from the mechanics that would be expected to contribute to injury risk, are due to a pain reduction mechanism employed by the PFP group. The runners with PFP may have tried to avoid poor mechanics to avoid pain. This seemed to be successful at the start of the run, when they did not report feeling pain; however, by the end of the run, there was an increase in motion that coincided with an increase in pain. Similarly, the runners with PFP had less peak knee flexion than controls. While an increase in knee flexion would indicate greater shock absorption and the opposite might be considered an injury risk, a decrease in knee flexion is thought to reduce patellofemoral compressive forces and therefore reduce pain for injured runners.27

Figure 4. IR = internal rotation, ER = external rotation. Reprinted with permission from reference 29.
In conclusion, any examination of the mechanical effects of running in an exerted state is complicated by various definitions and methods of generating fatigue in runners. Studies that examine a normal training run may be in the best position to determine the typical exercise effects on lower extremity mechanics. With cross-sectional studies, the risk of injury cannot be determined; however, a trend toward mechanics associated with running injury risk has been observed for healthy athletes running in an exerted state. Injured runners, when in an exerted state, tend to adopt mechanics that may be protective against pain. Overall, there are exercise-related changes in lower extremity mechanics associated with an exerted state that could be even more pronounced when the duration or intensity of the run increases beyond what is considered typical.
Lauren Benson, MS, is a PhD candidate and Kristian O’Connor, PhD, is associate professor and chair of the Department of Kinesiology at the University of Wisconsin-Milwaukee.
- Walter SD, Hart LE, McIntosh JM, Sutton JR. The Ontario cohort study of running-related injuries. Arch Intern Med 1989;149(11):2561-2564.
- Taunton JE, Ryan MB, Clement DB, et al. A retrospective case-control injuries analysis of 2002 running. Br J Sports Med 2002;36(2):95-101.
- van Gent RN, Siem D, van Middelkoop M, et al. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br J Sports Med 2007;41(8):469-480.
- Taunton JE, Ryan MB, Clement DB, et al. A prospective study of running injuries: The vancouver sun run “in training” clinics. Br J Sports Med 2003;37(3):239-244.
- James SL, Jones DC. Biomechanical aspects of distance running injuries. In: Cavanagh PR, ed. Biomechanics of Distance Running. Champaign, IL: Human Kinetics; 1990:249-269.
- Thijs Y, De Clercq D, Roosen P, Witvrouw E. Gait-related intrinsic risk factors for patellofemoral pain in novice recreational runners. Br J Sports Med 2008;42(6):466-471.
- Barton CJ, Munteanu SE, Menz HB, Crossley KM. The efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome. Sports Med 2010;40(5):377-395.
- Hreljac A. Impact and overuse injuries in runners. Med Sci Sports Exerc 2004;36(5):845-849.
- Kannus P. Etiology and pathophysiology of chronic tendon disorders in sports. Scand J Med Sci Sports 1997;7(2):107-112.
- Nigg BM. Biomechanical aspects of running. In: Nigg BM, ed. Biomechanics of Running Shoes. Champaign, IL: Human Kinetics; 1986:1-25.
- Nigg BM, Bahlsen AH, Denoth J, et al. Factors influencing kinetic and kinematic variables in running. In: Nigg BM, ed. Biomechanics of Running Shoes. Champaign, IL: Human Kinetics; 1986:139-160.
- Hintermann B, Nigg BM. Pronation in runners – implications for injuries. Sports Med 1998;26(3):169-176.
- Powers CM, Ward SR, Chen YJ, et al. Effect of bracing on patellofemoral joint stress while ascending and descending stairs. Clin J Sport Med 2004;14(4): 206-214.
- Scott SH, Winter DA. Internal forces at chronic running injury sites. Med Sci Sports Exerc 1990;22(3): 357-369.
- Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech 2008;23(2):203-211.
- Stefanyshyn DJ, Stergiou P, Lun VMY, et al. Knee angular impulse as a predictor of patellofemoral pain in runners. Am J Sports Med 2006;34(11):1844-1851.
- Powers CM. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J Orthop Sports Phys Ther 2010;40(2):42-51.
- Boling MC, Padua DA, Marshall SW, et al. A prospective invesitgation of biomechanical risk factors for patellofemoral pain syndrome. Am J Sports Med 2009;37(11):2108-2116.
- Enoka RM, Stuart DG. Neurobiology of muscle fatigue. J Appl Physiol 1992;72(5):1631-1648.
- Gandevia SC. Spinal and supraspinal factors in human muscle fatigue. Physiol Rev 2001;81(4): 1725-1789.
- Weir JP, Beck TW, Cramer JT, Housh TJ. Is fatigue all in your head? A critical review of the central governor model. Br J Sports Med 2006;40(7): 573-586.
- Ament W, Verkerke GJ. Exercise and fatigue. Sports Med 2009;39(5): 389-422.
- Lucci S, Cortes N, Van Lunen B, et al. Knee and hip sagittal and transverse plane changes after two fatigue protocols. J Science Med Sport 2011;14(5): 453-459.
- Nummela AT, Heath KA, Paavolainen LM, et al. Fatigue during a 5-km running time trial. Int J Sports Med 2008;29(9): 738-745.
- Abt JP, Sell TC, Chu Y, et al. Running kinematics and shock absorption do not change after brief exhaustive running. J Strength Cond Res 2011;25(6):1479-1485.
- Dierks TA, Davis IS, Hamill J. The effects of running in an exerted state on lower extremity kinematics and joint timing. J Biomech 2010;43(15):2993-2998.
- Dierks TA, Manal KT, Hamill J, Davis IS. Lower extremity kinematics in runners with patellofemoral pain during a prolonged run. Med Sci Sports Exerc 2011;43(4):693-700.
- Bazett-Jones DM, Cobb SC, Huddleston WE, et al. Effect of patellofemoral pain on strength and mechanics after an exhaustive run. Med Sci Sports Exerc 2013;45(7):1331-1339.
- Benson LC, O’Connor KM. The effect of exertion on joint kinematics and kinetics during running using a waveform analysis approach. J Appl Biomech 2015;31(4):250-257.
- Chan-Roper M, Hunter I, Myrer JW, et al. Kinematic changes during a marathon for fast and slow runners. J Sports Sci Med 2012;11(1):77-82.
- Derrick TR, Dereu D, McLean SP. Impacts and kinematic adjustments during an exhaustive run. Med Sci Sports Exerc 2002;34(6):998-1002.
- Hardin EC, Van den Bogert AJ, Hamill J. Kinematic adaptations during running: Effects of footwear, surface, and duration. Med Sci Sports Exerc 2004;36(5)838-844.
- Valiant GA. Transmission and attenuation of heelstrike accelerations. In: Cavanagh PR, ed. Biomechanics of Distance Running. Champaign, IL: Human Kinetics; 1990:225-247.
- Derrick TR, Hamill J, Caldwell GE. Energy absorption of impacts during running at various stride lengths. Med Sci Sports Exerc 1998;30(1):128-135.
- Mercer JA, Bates BT, Dufek JS, Hreljac A. Characteristics of shock attenuation during fatigued running. J Sports Sci 2003;21(11):911-919.
- Collins MH, Pearsall DJ, Zavorsky GS, et al. Acute effects of intense interval training on running mechanics. J Sports Sci 2000;18(2):83-90.
- Hanley B, Smith LC, Bissas A. Kinematic variations due to changes in pace during men’s and women’s 5 km road running. Int J Sports Sci Coach 2011;6(2):243-252.
- Williams KR, Snow R, Agruss C. Changes in distance running kinematics with fatigue. Int J Sport Biomech 1991;7(2):138-162.
- Mizrahi J, Verbitsky O, Isakov E, Daily D. Effect of fatigue on leg kinematics and impact acceleration in long distance running. Human Move Sci 2000;19(2):139-151.
- Nicol C, Komi PV, Marconnet P. Effects of marathon fatigue on running kinematics and economy. Scan J Med Sci Sports 1991;1(4):195-204.
- Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. J Orthop Sports Phys Ther 1987;9(4):160-165.
- VanGheluwe B, Madsen C. Frontal rearfoot kinematics in running prior to volitional exhaustion. J Appl Biomech 1997;13(1):66-75.