 High relapse rate from preseason injuries presents significant challenge for athletes and sports teams.
High relapse rate from preseason injuries presents significant challenge for athletes and sports teams.
By Keith Loria
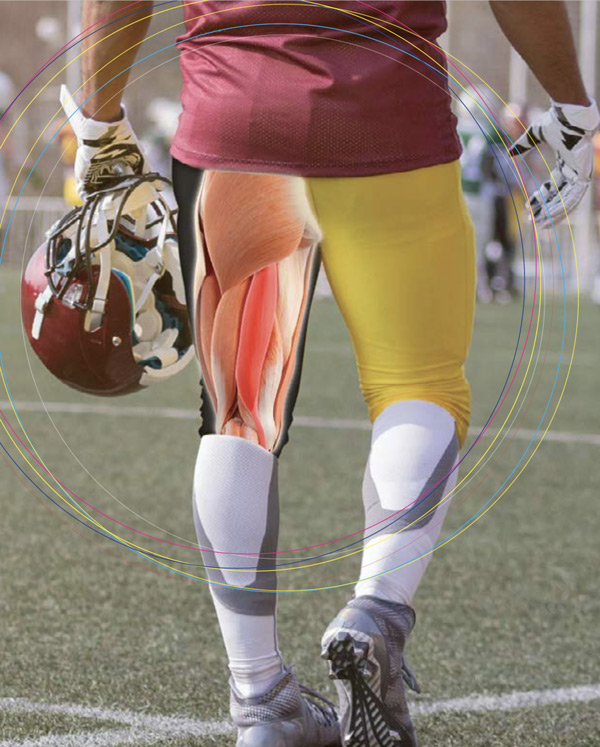
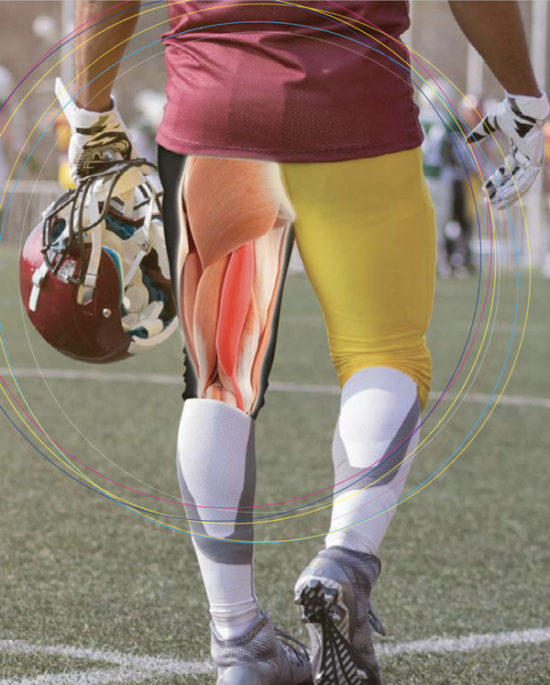
Hamstring strain injuries are among the most common in sports, often leading to recurring problems or future injury. Marcus Elliott, director of P3 Applied Sports Science and a former muscle-injury specialist for the National Football League’s New England Patriots, conducted a 10-year analysis1 of hamstring strain injuries in football and reported that more than 50% of those that occurred during the preseason became further problematic throughout the regular season. This high relapse rate is a challenge for sports medicine specialists and has a significant impact on athletes and sport teams.
Matthew Bourne, department of rehabilitation, nutrition, and sport at the La Trobe Sport and Exercise Medicine Research Centre, Melbourne, Australia, led a study2 that looked at how strengthening exercises worked to prevent hamstring injury. “Enough evidence suggests that the acute responses and chronic adaptations to training with different hamstring exercises are heterogeneous,” he said. “Muscle activation may be an important determinant of training-induced hypertrophy; however, contraction mode appears to be the largest driver of architectural changes within the hamstrings.”
Based on the results of the study, which was published in Sports Medicine in February, Bourne and coauthors reported that improved understanding of this empiric evidence will someday enable practitioners to make better-informed decisions around exercise selection for the prevention or treatment of hamstring strain injury. Bourne thinks that some clinical guidelines for hamstring prevention and rehabilitation are based on anecdotal information: “We wanted to go through the literature and try to provide a bit of an evidence-based approach to strength training,” Bourne said. “What we know is that there’s very good evidence for eccentric conditioning to prevent hamstring injury.”
Bourne cited other studies3 that have proved that eccentric knee–flexor conditioning decreases the risk of hamstring strain injury when compliance is adequate, adding that these benefits are more likely to be at least partly mediated by 1) increases in biceps femoris long-head fascicle length, 2) possibly a rightward shift in the angle of peak knee–flexor torque, and 3) improvements in eccentric knee-flexor strength—although other adaptations may contribute. He noted in his study that athletes with short fascicles were 4 times more likely to tear their hamstrings; a 1-cm increase in fascicle length reduces the risk of a hamstring injury by approximately 74%.2
Physical therapy modalities

iStockphoto.com 518917755
John Sauer PT, DPT, OCS, endurance program co-manager for Athletico, La Grange Park, IL, said that, although certain physical therapy modalities, such as moist heat, electrophysiologic agents, and therapeutic ultrasound, can be an effective adjunct to treatment in early pain-management stages, he has found that the earlier athletes are able to return to more active interventions, the faster they tend to recover. “I have yet to see a convincing study on improved hamstring muscle healing from modalities,” he said. “I tend to avoid use of modalities with this patient population.”
Timothy F. Tyler MS, PT, ATC, physical therapist at the Nicholas Institute of Sports Medicine and Athletic Trauma at Lenox Hill Hospital, New York, NY, has treated lacrosse players through the years, and notes that hamstring injuries are the most prevalent ones in the sport. Tyler usually has about 4 to 6 weeks for in-season injury to heal so that the athlete can resume playing—but there’s often just one chance of doing that.
“If they [have] a reoccurrence during that same season, it’s very hard to get them back on the field,” he said. For the first phase of treatment, Tyler prescribes rest, ice compression, and isometric contractions, but not stretching the injured muscle. The regimen aims to preserve the available range of motion but not to take it past its passive endpoint.
For the second phase of treatment, Tyler looks at more isotonic and dynamic exercises, starting to strengthen the muscle in the lengthened state with hip and the knee. The third, final phase includes maximum eccentric strengthening in length and speed to prevent recurrences.
Bourne agrees that the most effective methods include strengthening exercises and conditioning as early as possible in the process, and are vital to rehabilitation.
Preventive steps
Emilia Ravski, MD, sports medicine physician with Hoag Orthopedic Institute, Irvine, CA, said the recent focus has been on injury prevention. To prevent injury, she shared, it is important to identify the many causes that can predispose an athlete to hamstring injury. Such factors include prior hamstring injury, training volume and errors, dysfunctional movement patterns, muscular strength imbalance, and lack of neuromuscular control. Although an athlete’s injury history cannot be changed, modifiable intrinsic and extrinsic risk factors should be addressed, Ravski noted. These include any necessary adjustments to training regimen and volume to avoid overloading the hamstring.
“In addition, a comprehensive functional assessment can elucidate dysfunctional movement patterns that may predispose one to a hamstring injury and should include evaluation of core stability, hip range of motion, quad flexibility and hamstring strength,” Ravski said. “Lastly, the pathologic process of injury begins prior to the onset of pain, thus minimizing biomechanical risk factors in combination with proper training should be emphasized. Early detection of symptoms is also very important as delayed treatment can lead to prolonged recovery.”
Over the long term, Sauer revealed, there is some good evidence regarding performance of Nordic lunges for injury prevention. For more general strength or conditioning work, an appropriately progressed squatting or deadlifting program can be helpful for a balanced approach to lower-extremity strengthening in athletic populations. “Additionally, I generally have my runners stay consistent with eccentric, single-leg windmill exercises to maintain good control with varied positions of the hip,” he said. “When we look at the function of the hamstring, it has a major role in deceleration of the leg with higher-speed running and kicking, so training it with control through full lengthening cycles is critical for avoiding recurrent strains.”
The rise of restorative medicine
Brian M. Grawe, MD, assistant professor of sports medicine and shoulder reconstruction in the Department of Orthopaedic Surgery and Sports Medicine at the University of Cincinnati College of Medicine, said the biggest buzz regarding hamstring injury today centers on restorative medicine. “Athletes are always looking for an advantage and we, as sports medicine doctors, are always trying to provide cutting-edge treatment options so that players can get back onto the field faster,” he said. “Restorative medicine comes in many varieties, but for hamstring injuries, it means biologic therapy to help heal the muscle and tendon injury.” This often includes growth factors and stem-cell therapies; although currently experimental, these options offer the potential for scar-free healing and shortened recovery times.
Sound rehab program
Newer treatment trends—particularly in soccer and running populations, where hamstring injuries are highly prevalent—increasingly focus on eccentric hamstring control, dynamic warmup exercises, and dry needling. “Dry needling is one passive intervention that is picking up more steam, which is the use of a needle to elicit a local twitch response from insertion into trigger points in the muscle tissue,” Sauer said. “I do not perform dry needling personally, as evidence on both trigger points and consistent effects of dry needling still needs further development; however, many athletes note a positive response.”
“Both [eccentric exercises and dry needling] are very effective,” said Grawe, “and [are] my first-line treatment for those athletes with acute hamstring injuries.” He noted that eccentric exercises can efficiently and safely build muscle strength following injuries, as the muscle is lengthening—similar to “negatives” on a biceps curl. Dry needling, he added, increases blood flow to the muscle and promotes healing. For hamstring strengthening, Grawe typically recommends a progression toward higher-velocity strengthening and reaction in lengthened positions, including eccentric strengthening with single-leg forward leans with medicine ball, single-leg dead lifts with dumbbells, single-leg bridge curls on a physioball, resisted-running foot catches, and Nordic curls.*
*Editor’s note: Other recently developed interventions for hamstring strengthening have spent time in the limelight. They include instrument-assisted soft-tissue mobilization (such as the Graston Technique® [http://www.grastontechnique.com] and Astym® [https://astym.com] brands) and cupping, a staple of the US swim team in the 2016 summer Olympics in Rio de Janeiro, Brazil.
Sauer recently worked with a high school sprinter 1 year post-hamstring strain, who had had partial success with a trial of physical therapy and was able to return to normal daily activities, even though he still had increased pain upon squatting and during high-speed running. Initial treatments for this sprinter included manual hamstring pin/stretch; the Graston Technique® applied to the medial hamstring; bridging with emphasis on gluteal activation; and prone hamstring isometrics at 90°. Emphasis was on avoidance of pain with all exercises. Sauer progressed the rehabilitation to single-leg bridging, multi-angle bridging/bridge walkouts, lateral band walks, Nordic lunges, “good mornings”, squat retraining, eccentric single-leg windmills, 3 cone taps, and independent soft-tissue work with foam roll/tennis ball, initiated over the following weeks.
“The patient was seen for 8 visits, over the course of 5 weeks, and the pain decreased from 6 [on a scale of 1 to] 10 with sprinting and squatting to 0 [on a scale of 1 to] 10, with symmetrical gluteal and hamstring [delayed-onset muscle soreness] on days after heavy squatting or sprinting,” Sauer said. “At time of discharge, he was not at his previous level of short distance times… which was attributed to lack of training volume over the prior 12 months.”
Bourne hopes that, in the future, clinicians realize there is strong evidence for single-joint eccentric movements like the Nordic hamstring exercise, which continues to be one of the most-debated exercises in the sports medicine industry.
Keith Loria is a freelance medical writer.
- Elliott MC, Zarins B, Powell J, Kenyon C. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843-50.
- Bourne MN, Timmins RG, Opar DA, et al. An evidence-based framework for strengthening exercises to prevent hamstring injury. Sports Med. 2018;48 (2):251-267.
- Ekstrand J, Walden M, Hagglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA Elite Club injury study. Br J Sports Med. 2016;50(12):731–7.