 By David Beck, MD, Justin Kane, MD, and David Pedowitz, MD
By David Beck, MD, Justin Kane, MD, and David Pedowitz, MD
Given that older women are at increased risk for osteoporosis, an increased incidence of fifth metatarsal fractures with increasing age in women suggests that such injuries could serve as an early point of entry into osteoporosis treatment and fracture prevention.
Fractures of the fifth metatarsal bone are a common injury encountered not only in the offices of foot and ankle specialists, but also frequently in primary care, sports medicine, and general orthopedic settings. In fact, multiple reports suggest fractures of the fifth metatarsal are the most common metatarsal fracture.1-5 Although it is a common injury, the literature on the epidemiology of fifth metatarsal fractures in large diverse populations has been scarce. Most studies on fifth metatarsal fractures have been performed in small European populations or have focused on specific populations such as athletes, dancers, and military personnel.1-7
A recent study from our institution looked at 2281 consecutive metatarsal fractures in a tertiary care subspecialty referral setting to investigate the epidemiology of fifth metatarsal fractures in the general population.8 A particularly interesting finding of the study was that an increased incidence of fifth metatarsal fractures was correlated with increasing age in women. Given that older women are at increased risk for osteoporosis, might these fractures be useful as a proxy for identifying and implementing appropriate therapies in patients at risk for osteoporosis?
Diagnosis and classification
British orthopedic surgeon Sir Robert Jones originally described fifth metatarsal fractures in 1902 in the Annals of Surgery. Jones’ interest in the topic was spurred by having the misfortune of sustaining the injury himself while dancing at a military garden party. Only after treating himself as a patient did Jones write in his first publication on the topic that he could “recall many cases which had come to me with similar symptoms arising from transmission of body weight to a foot during the position of equinovarus.” Jones had recognized the commonality of this fracture pattern and set out to describe it in detail. His future work on these fractures gave rise to the eponym for fractures of the base of the fifth metatarsal: the Jones fracture.
Fractures of the fifth metatarsal can be classified by location. As with all metatarsal fractures, fifth metatarsal fractures can first be categorized into three main locations: base, shaft, and head. Proximal fifth metatarsal fractures can be further classified into three zones.4,6,10 Zone 1 fractures (pseudo-Jones) are avulsion fractures of the cancellous tuberosity. This area of bone includes the insertions of the peroneus brevis tendon and lateral plantar fascia. These fractures are usually secondary to an inversion injury.11 Zone 2 fractures (true Jones) occur distal to the tuberosity at the metaphyseal-diaphyseal junction and do not extend past the fourth-fifth intermetatarsal articulation. These typically occur secondary to an adduction force on a plantar flexed foot, just as Jones initially described. Finally, zone 3 injuries occur at the proximal diaphysis, distal to the proximal ligaments. These are thought to occur usually as stress fractures occurring secondary to repetitive activity; fractures in this region are common in athletes and military workers. Another specific pattern of fracture at the distal diaphysis of the fifth metatarsal has been labeled the dancer’s fracture.7 This is usually a spiral oblique fracture traveling from a distal-lateral location to a proximal-medial location and is sustained after a rotational force is applied to an axially loaded plantar flexed foot.11

Figure 1. Stratification of fifth metatarsal fractures with fractures denoted by a white arrow. (A) Avulsion fracture of the base of the fifth metatarsal (zone 1; pseudo-Jones). (B) Jones (zone 2) fracture. (C) Zone 3 fracture of the base of the fifth metatarsal. (D) Dancer’s fracture. (E) Transverse fifth metatarsal shaft fracture. (F) Stress fracture of the fifth metatarsal shaft. (Reprinted with permission from reference 8.)
Several previous studies have looked at the epidemiology of all metatarsal fractures, but few have examined the epidemiology of all types of fifth metatarsal fractures in the general US population. Cakir et al assessed 400 metatarsal fractures in 322 consecutive patients in a European population. They found the fifth metatarsal accounted for 56% of metatarsal fractures.2 Similarly, Petrisor et al retrospectively examined 355 patients with 411 metatarsal fractures in an adult European population and found that fifth metatarsal fractures accounted for 68% of the injuries.1 A similar pattern is also seen in pediatric populations, with fifth metatarsal fractures accounting for 45% of all metatarsal fractures.5 To our knowledge, ours was the first study to look at the epidemiology of all types of fifth metatarsal fractures in a general US population.
Our research
To investigate the epidemiology of fifth metatarsal fractures in the general population at our institution, Kane et al retrospectively collected data on 2281 patients with metatarsal fractures seen between June 1, 2005, and December 30, 2010. Radiographic review further identified 1275 patients (59%) who were treated for isolated fifth metatarsal fractures. These fractures were then further classified by location of fracture: base (zone 1, 2, or 3), shaft, dancer’s stress, or head fracture. Using patient records, the authors then reviewed data on age, gender, comorbidities, and mechanism of injury.
The study successfully elucidated the epidemiology of the location of fifth metatarsal fractures. Most of the fractures in the study were avulsions of the base of the fifth metatarsal, which accounted for 51% of the fractures. Shaft fractures were the next most common fracture pattern, followed by zone 2 and dancer’s fractures, accounting for 16.8%, 13.6%, and 11.1%, respectively. An arguably more interesting finding occurred when fracture location was correlated with gender. The vast majority of avulsion fractures at the base of the fifth metatarsal (74%) and dancer’s fractures (84%) occurred in women.
As discussed earlier, each fracture pattern has a proposed mechanism of injury. In this retrospective study, Kane et al reviewed the mechanism of each injury and correlated it with the fracture pattern observed on radiographs. The mechanisms in this study were categorized as twisting, fall, crush, indirect trauma, or atraumatic. Twisting injuries accounted for 64.6% of zone 1 fractures. However, a twisting mechanism accounted for the majority of all other fifth metatarsal fractures as well.
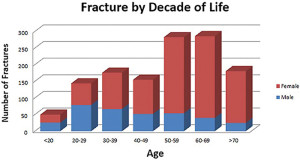
Figure 2. In men, the incidence of fifth metatarsal fractures peaks in the third decade of life. In women, there is a peak in the seventh decade of life. The majority of fifth metatarsal fractures are seen in the sixth and seventh decades of life and are predominantly sustained by women. (Reprinted with permission from reference 8.)
Another important finding of the study emerged when we examined the age distribution of patients presenting with fifth metatarsal fractures. The distribution of these fractures had a bimodal pattern across the general population, with peaks in both the fourth decade and the sixth/seventh decades. Fifth metatarsal fractures continued to increase with each decade of life until the eighth decade. When stratifying for gender, it was clear that fifth metatarsal fractures in men are more common earlier in life and in women later in life. Men were more likely to experience a fracture in their third decade, whereas women had a great increase in fractures in the sixth and seventh decades. In fact, fractures in women alone were the reason for the positive correlation between age and fracture incidence.
Osteoporosis implications
To date, Kane et al is the largest cohort study examining fifth metatarsal fractures. The study reinforced that fifth metatarsal fractures are the most common metatarsal fracture. It illuminated that avulsion fractures are the most common type of fifth metatarsal fractures. However, the most interesting and potentially useful piece of information to come from this study was the steady increase in fifth metatarsal fractures with increasing age in women. The fact that these fractures increase with age in women but decrease with age in men may very well be secondary to an increase in osteopenia and osteoporosis in women, who are known to have a steady age-related decrease in bone mineral density (BMD) that is not typically seen in men.
Osteoporosis and fracture prevention has become an important topic in the US, given the continued expansion of the physically active aging population. The most common osteoporosis-related fractures, or fragility fractures, are vertebral, proximal femoral, and distal forearm fractures. Approximately two million fragility fractures occur in the US every year and incur approximately $17 billion in healthcare costs.16 Any patient experiencing one of these fractures has an 86% increased risk of experiencing another.13 As the population ages, the disease burden will increase, and fractures, as well as the related costs, are expected to grow by 50% by 2025, with more than three million fractures and $25 billion in costs.17 At this rate, early identification and fracture prevention will be of utmost importance.
 In recent years there has been a movement in orthopedics, in collaboration with other disciplines, to increase the role of the orthopedic surgeon in identifying patients at risk of osteoporosis and initiating the appropriate workup and treatment or referral. This is the reason the American Orthopaedic Association launched the “Own the Bone” campaign.12 This program is aimed at increasing the responsibility of orthopedists in closing the osteoporosis treatment gap. Some hospitals have gone as far as creating a Fracture Liaison Service, which automatically identifies and refers anyone with an osteoporosis-related fracture for bone health evaluation, secondary fracture prevention, and osteoporosis intervention.13 Lower-energy proximal humerus and distal radius fractures are already being used by upper extremity specialists as indications for referral for an osteoporosis work-up.14,15 Fifth metatarsal fractures may be a proxy in the foot and ankle specialty that helps to identify these at-risk patients.
In recent years there has been a movement in orthopedics, in collaboration with other disciplines, to increase the role of the orthopedic surgeon in identifying patients at risk of osteoporosis and initiating the appropriate workup and treatment or referral. This is the reason the American Orthopaedic Association launched the “Own the Bone” campaign.12 This program is aimed at increasing the responsibility of orthopedists in closing the osteoporosis treatment gap. Some hospitals have gone as far as creating a Fracture Liaison Service, which automatically identifies and refers anyone with an osteoporosis-related fracture for bone health evaluation, secondary fracture prevention, and osteoporosis intervention.13 Lower-energy proximal humerus and distal radius fractures are already being used by upper extremity specialists as indications for referral for an osteoporosis work-up.14,15 Fifth metatarsal fractures may be a proxy in the foot and ankle specialty that helps to identify these at-risk patients.
Although we hypothesize that decreased BMD in the elderly population is the reason for an increased incidence of fifth metatarsal fractures, our study did not measure BMD in these patients. However, previous research has adequately documented a direct relationship between fractures of the foot and low levels of BMD.
Hasselman et al18 studied a cohort of 9704 elderly women for a mean of 10.2 years. On the initial visit, each patient’s BMD was measured. The study found a high incidence of both ankle and foot fractures (3.1 and 3 per 1000 woman years, respectively), but found that decreased BMD correlated only to foot fractures. Ankle fractures happened at an equal rate between women with decreased BMD and those with normal BMD, suggesting a significant traumatic mechanism versus an osteopenic fragility fracture as the injury source. Of all foot fractures, 88.5% involved a metatarsal and 56.9% involved the fifth metatarsal.18
Another study demonstrated that age-matched women with metatarsal fractures after minor trauma had lower lumbar BMD compared with that of healthy women.19 This study showed that metatarsal fracture patients had BMD similar to age-matched patients with a distal radius fracture, a well-documented fragility fracture. However, the metatarsal fracture patients were younger at the time of fracture, suggesting it could be an earlier marker for osteopenia.19
While osteopenia is a one of the causes of increased fracture rate in the elderly population, the foot and ankle specialist must be aware of other potential risks for increased rates of metatarsal fractures in this group. Other factors reported to be associated with foot fractures are insulin-dependent diabetes, use of seizure medications, history of falls, poor depth perception, hyperthyroidism, and use of benzodiazepines.18-20 Diabetes may be related to foot fractures for several reasons, including diabetic osteopathy as well as peripheral neuropathy.21 A history of falls and trouble with depth perception increase the risk of foot trauma for obvious reasons. However, the increased risk of fracture with benzodiazepine use does not seem to be related to increased fall risk, and further research should be done to investigate that reported correlation.18 For a multitude of reasons, elderly patients have an increased risk of fifth metatarsal fractures. Therefore, practitioners must take a thorough history of any patient presenting with a metatarsal fracture.
Conclusion
While more research on osteoporosis in patients presenting with fifth metatarsal fractures still needs to be done, the epidemiologic study by Kane et al demonstrates that these fractures occur with increasing incidence in a population known to have an increased incidence of osteoporosis. An elderly man or women who comes in with a fifth metatarsal fracture is presenting with a relatively low-cost and low-morbidity injury, as most can be treated effectively with surgery.21-23 However, if this injury is indicative of an underlying bone density issue, it could serve as an early point of entry into osteoporosis treatment and secondary fracture prevention protocols. Thus, physicians treating these injuries may want to consider referral to an appropriate resource for osteoporosis intervention before that patient experiences a hip fracture or a vertebral fracture, which have higher associated costs and morbidity.
David Beck, MD, is a third-year orthopedic surgery resident at Thomas Jefferson University Hospital in Philadelphia, PA. Justin Kane, MD, is a former orthopedic surgery resident at Thomas Jefferson University Hospital and is currently completing a Foot and Ankle Surgery Fellowship at Baylor University Medical Center in Dallas, TX. David Pedowitz,MD, is a fellowship-trained orthopedic foot and ankle specialist and an assistant professor of orthopaedic surgery at Thomas Jefferson Medical College.
- Petrisor BA, Ekrol I, Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int 2006;27(3):172-174.
- Cakir H, Van Vliet-Koppert ST, Van Lieshout EMM, et al. Demographics and outcome of metatarsal fractures. Arch Orthop Trauma Surg 2011;131(2):241-245.
- Clapper MF, O’Brien TJ, Lyons PM. Fractures of the fifth metatarsal: analysis of a fracture registry. Clin Orthop Relat Res 1995;(315):238-241.
- Fetzer GB, Wright RW. Metatarsal shaft fractures and fractures of the proximal fifth metatarsal. Clin Sports Med 2006;25(1):139-150.
- Owen RJT, Hickey FG, Finlay DB. A study of metatarsal fractures in children. Injury 1995;26(8):537-538.
- Torg JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth metatarsal distal to the tuberosity. Classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am 1984;66(2):209-214.
- O’Malley MJ, Hamilton WG, Munyak J. Fractures of the distal shaft of the fifth metatarsal “dancer’s fracture.” Am J Sports Med 1996;24(2):240-243.
- Kane JM, Sandrowski K, Saffel H, et al. The epidemiology of fifth metatarsal fracture. Foot Ankle Spec 2015 Feb 9. [Epub ahead of print]
- Jones R. Fracture of the base of the fifth metatarsal bone by indirect violence. Ann Surg 1902;35(6):697-700.
- Egol K, Walsh M, Rosenblatt K, et al. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot Ankle Int 2007;28(5):581-583.
- Egol KA, Koval KJ, Zuckerman JD. Fractures of the midfoot and forefoot. In: Handbook of Fractures. 5th ed. Wolters Kluwer Health; 2015: 536-539.
- Bunta AD. It is time for everyone to own the bone. Osteoporos Int 2011;22(Suppl 3):477-482.
- Miller AN, Lake AF, Emory CL. Establishing a fracture liaison service: an orthopaedic approach. J Bone Joint Surg Am 2015;97(8):675-681.
- Gutowski CJ, Ilyas AM. Evaluation and medical management of fragility fractures of the upper extremity. Orthop Clin North Am 2014;45(2):233-243.
- Rozental TD, Makhni EC, Day CS, Bouxsein ML. Improving evaluation and treatment for osteoporosis following distal radial fractures. J Bone Joint Surg 2008;90(5):953-
- Ekman EF. The role of the orthopaedic surgeon in minimizing mortality and morbidity associated with fragility fractures. J Am Acad Orthop Surg 2010;18(5):278-
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 2007;22(3):465-
- Hasselman CT, Vogt MT, Stone KL, et al. Foot and ankle fractures in elderly white women. J Bone Joint Surg Am 2003:85(5):820-824.
- Varenna M, Binelli L, Zucchi F, et al. Is the metatarsal fracture in postmenopausal women an osteoporotic fracture? A cross-sectional study on 113 cases. Osteoporos Int 1997;7(6):558-563.
- Seeley DG, Kelsey J, Jergas M, Nevitt MC. Predictors of ankle and foot fractures in older women. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 1996;11(9):1347-1355.
- Cundy TF, Edmonds ME, Watkins PJ. Osteopenia and metatarsal fractures in diabetic neuropathy. Diabet Med 1985;2(6)461-464.
- Aynardi M, Pedowitz DI, Saffel H, et al. Outcome of nonoperative management of displaced oblique spiral fractures of the fifth metatarsal shaft. Foot Ankle Int 2013;34(12):1619-
- Egol K, Walsh M, Rosenblatt K, et al. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot Ankle Int 2007;28(5):581-
- Polzer H, Polzer S, Mutschler W, Prall WC. Acute fractures to the proximal fifth metatarsal bone: Development of classification and treatment recommendations based on the current evidence. Injury 2012;43(10):1626-








