 Clinicians and researchers are increasingly utilizing exercise protocols focused on improving proprioception, range of motion, and strength to influence the more active and functional deficits that have been associated with chronic ankle instability in the literature.
Clinicians and researchers are increasingly utilizing exercise protocols focused on improving proprioception, range of motion, and strength to influence the more active and functional deficits that have been associated with chronic ankle instability in the literature.
By Mark A. Feger, MEd, ATC, and Jay Hertel, PhD, ATC
Ankle sprains are the most common musculoskeletal injury1-3 and up to 40% of patients who sprain an ankle develop chronic ankle instability (CAI).4 CAI is characterized by recurrent sprains, multiple episodes of the ankle giving way, persistent symptoms, and diminished self-reported function for at least one year following a significant ankle sprain.5 Additionally, seven out of every 10 people who sprain an ankle are unable to maintain their previous level of physical activity, and many of these patients may develop post-traumatic osteoarthritis.6,7
Not only do ankle sprains have tremendous implications for each individual patient, but ankle sprains are also a large financial burden worldwide.8,9 Since recurrent ankle sprains in patients with CAI account for a large proportion of all ankle sprains, it is very important for clinicians to understand the pathomechanics that predispose patients with CAI to repetitive injury. Furthermore, therapeutic exercise should be aimed specifically at improving the functional pathomechanics identified in patients with CAI to eliminate potential predispositions to future injury.
CAI is a heterogeneous condition with a large spectrum of associated impairments that range from passive proprioceptive deficits to more active alterations in jump-landing and cutting mechanics.10 It is widely accepted that many of the less functional impairments in proprioception, range of motion (ROM), and strength are likely influencing the more active deficits identified in the literature of altered kinematics,11-15 kinetics13,16,17 and muscle activity 13,18,19 during walking, running, and jump landing. Our purposes in this review are to highlight the pathomechanics on the functional end of the measurement spectrum in CAI patients (Table 1) and the current literature on therapeutic exercise programs that specifically address functional limitations in CAI patients.
Functional pathomechanics and CAI
Altered postural control has been identified during static20-22 and dynamic23,24 balance tasks in patients with CAI. Additionally, decreased postural stability has been identified as a potential risk factor for sustaining an initial or recurrent ankle sprain.21 Static balance deficits are usually identified with spatiotemporal measures requiring instrumentation, such as time-to-boundary calculations,20 whereas dynamic balance deficits can be detected clinically with the star excursion balance test (SEBT) (Figure 1).25,26 We recently identified that patients with CAI exhibit significantly less anterior tibialis and total lower extremity muscle activity while performing both single-limb balance and the SEBT exercises compared with healthy individuals.19
During walking gait, patients with CAI demonstrate moderate increases in ankle inversion just prior to and following initial contact.12,16 The increased inversion positioning following initial contact is associated with increased lateral loading during stance.16 To improve ankle joint position prior to ground contact, patients with CAI activate the peroneus longus prior to ground contact, whereas their healthy counterparts do not activate the peroneus longus until the initiation of pronation during midstance.18 Improper foot position prior to ground contact is theorized to play a role in the frequent rate of recurrence or the repetitive sensations of giving way in this pathological population.
While jogging, patients with CAI exhibit less peak dorsiflexion (~5° less) during stance15 than uninjured individuals, as well as less coordinated foot and ankle joint coupling.14 Specifically, patients with CAI have more inversion and shank external rotation while walking and jogging.14 The decreased dorsiflexion motion identified by Drewes et al15 during the stance phase of jogging is similar to the findings of Brown et al11 during the swing phase of running, in which patients with CAI demonstrated decreased vertical foot-floor clearance; both findings represent a period of increased plantar flexion during the gait cycle. Collectively, a more plantar flexed and inverted foot position, as well as the decreased foot-floor clearance, may predispose individuals with CAI to subsequent ankle sprains during jogging and running.
Similar results have been obtained during jump-landing tasks. Delahunt et al13 found patients with CAI have greater inversion (~4° more inverted) than healthy individuals prior to initial contact during a single-leg drop jump, and that they are less dorsiflexed following initial contact (~5° more plantar flexed). The increased inversion positioning identified prior to initial contact was likely related to the decreased peroneus longus muscle activity identified during that phase of landing.13
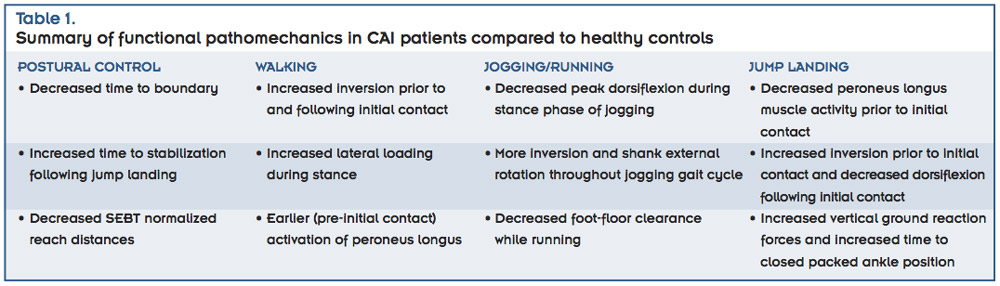 The less dorsiflexed positioning following initial contact was associated with increased ground reaction forces and a slower time to the more stable closed packed ankle position,13 the point at which there is maximal joint stability due to inert structures such as congruency of bony surfaces and taut ligaments. Furthermore, Gribble et al 27 identified decreased knee flexion positioning at ground contact and increased time to stabilization after ground contact in CAI patients during single-limb jump landing following a maximal vertical jump. Collectively, these jump-landing studies indicate that CAI patients land on a more rigid limb than healthy individuals, which may increase demand on the static and dynamic lateral ankle stabilizers.
The less dorsiflexed positioning following initial contact was associated with increased ground reaction forces and a slower time to the more stable closed packed ankle position,13 the point at which there is maximal joint stability due to inert structures such as congruency of bony surfaces and taut ligaments. Furthermore, Gribble et al 27 identified decreased knee flexion positioning at ground contact and increased time to stabilization after ground contact in CAI patients during single-limb jump landing following a maximal vertical jump. Collectively, these jump-landing studies indicate that CAI patients land on a more rigid limb than healthy individuals, which may increase demand on the static and dynamic lateral ankle stabilizers.
Emerging themes are expressed in the literature regardless of the type of functional impairment identified in CAI patients. Patients with CAI have decreased postural stability during static and dynamic balance as well as following jump-landing tasks. Increased inversion and plantar flexion positioning are evident during walking, jogging, and jump landing, whereas alterations in muscle activity appear to be task dependent.
Effects of therapeutic exercise
A wide range of therapeutic interventions has been implemented for the treatment of pathomechanics in patients with CAI, however, we focus on the effects of therapeutic exercise that specifically targets improving balance and gait.
A systematic review by Loudon et al 28 indicates that rehabilitation can improve postural control in patients with ankle instability. In the review, 28 the authors included studies of very simplistic balance training interventions as well as more comprehensive rehabilitation programs, both of which are effective interventions for improving postural control. These results highlight that there may be multiple methods clinicians can use to improving balance in patients with CAI depending on the available resources and time available to work with a given patient.
Gauffin et al29 described an example of a more simplistic balance training intervention in terms of duration and exercise variety. However, they were able to demonstrate improved postural control in patients with functional ankle instability after eight weeks of ankle disc balance training for 10 minutes per day, five days per week.29 Another balance training program by Ross and Guskiewicz30 utilized single-leg foam balance, wobble board exercises, and resistance band kicks for 10 minutes per day, five days per week; they found that anterior-posterior and medial-lateral time to stabilization deficits could also be improved in patients with functional ankle instability following a four-week intervention. However, their results suggested that anterior-posterior stability can improve after two weeks, whereas medial-lateral stability may take as long as four weeks. 30 Clinicians should be aware that total ankle stability does not improve until both frontal and sagittal postural stability are achieved, and that patients with CAI may benefit from exercises that emphasize frontal plane stability. 30
Hale et al31 utilized a more comprehensive rehabilitation program that incorporated range of motion, strengthening, and neuromuscular training exercises. In this study,31 patients with ankle instability demonstrated a 10% improvement in self-reported function as measured by the foot and ankle disability index and 7% to 12% improvement in dynamic balance capabilities as measured with the SEBT following a four-week intervention. This study indicated that, not only can practitioners use the SEBT to identify dynamic balance deficits in patients with CAI, they can also use it to track postintervention improvements in dynamic balance.31
Two systematic reviews have indicated that neuromuscular training also prevents lateral ankle sprains effectively.28,32 The preventive effects are more pronounced in patients with a history of ankle sprain and in patients with prolonged neuromuscular training (more than two years).32 Most studies included in the reviews based neuromuscular training programs largely on balance training.32 The effective balance training programs had a few key characteristics of which clinicians should be aware.33-35 Each protocol was progressive, as participants began with a single-limb eyes-open balance condition on a firm stable surface and progressed to neuromuscular training exercises with more demanding constraints. Additionally, the protocols all incorporated a balance/wobble board (Figure 2) during later stages of the progression, and participants did each protocol for more than six weeks. A key contributor to the success of any intervention is compliance, and each of these protocols was implemented in a team sport environment to ensure maximal compliance.

Figure 3. Hop to stabilization task: anterior-posterior hop direction, medial-lateral hop direction, anteromedial-posterolateral hop direction, and respective directions for foam pad placement (descending order of images).
The effects of therapeutic exercise on walking, jogging, running, and jump-landing mechanics in patients with CAI are less well understood. In a 2009 randomized controlled trial McKeon et al36 analyzed the effects of four weeks of supervised balance training on walking and jogging gait parameters. The balance training protocol was a progressively challenging hop to stabilization (Figure 3) protocol that had previously been found effective for improving postural control in CAI patients.37 In the 2009 study36 the authors found significant improvements in self-reported function, but did not identify meaningful changes in inversion/eversion kinematics or shank rotation kinematics following the balance training intervention. However, they did identify improved joint coupling between the shank and rearfoot, indicating a more coordinated gait pattern.36 Furthermore, the authors analyzed ligamentous laxity before and after the balance training intervention and were able to demonstrate that the functional improvements in gait were due to changes in sensorimotor function as opposed to local changes in joint stability.36
It should be noted that the short-term (four weeks) intervention might not be an adequate duration to overcome compensatory gait patterns, or that perhaps a more comprehensive rehabilitation program that addresses range of motion, strength, balance, functional exercise, and gait retraining may be required to restore normal gait mechanics.
Up to this point there has not been a randomized controlled trial that has analyzed the effects of a more comprehensive rehabilitation program on walking, jogging, running, or jump-landing movement patterns in patients with CAI, but a recent case report has suggested the potential efficacy of such a program.38 O’Driscoll et al38 reported on the effects of a six-week progressive neuromuscular training program in a single patient with CAI. In this case report,38 the rehabilitation included strengthening exercises, postural stability, plyometrics, and speed/agility drills. Following the intervention, self-reported function and SEBT scores improved.38 Furthermore, the researchers were able to identify decreased ground reaction forces during walking and decreased plantar flexion during jump landing, indicating the potential efficacy of thorough rehabilitation programs for altering walking and jump-landing mechanics in patients with CAI.38
Clinicians should also be aware of a recent rehabilitation paradigm established by Donovan and Hertel39 that highlights a rehabilitation algorithm for addressing common limitations in patients with CAI. The authors emphasize the importance of assessing patients for each passive and active functional limitation and prescribing rehabilitation based on the identified limitations.39 This algorithm is extremely helpful for limitations associated with range of motion, strength, balance, and some more functional impairments.39 However, in a clinical setting, it may be difficult to assess for altered kinematics, kinetics, or muscle recruitment patterns while patients are walking, running, or landing from a jump. In these instances, it is increasingly important that clinicians be aware of the functional pathomechanics commonly observed in patients with CAI as well as effective therapeutic exercises to address the functional impairments.
Mark A. Feger, MEd, ATC, is a doctoral student and Jay Hertel, PhD, ATC, is the Joe Gieck Professor in Sports Medicine in the Department of Kinesiology at the University of Virginia in Charlottesville.
1. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: Summary and recommendations for injury prevention initiatives. J Athl Train 2007;42(2):311-319.
2. Waterman BR, Belmont PJ, Cameron KL, et al. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med 2010;38(4):797-803.
3. Waterman BR, Owens BD, Davey S, et al. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am 2010;92-A(13):2279-2284.
4. Gerber JP, Williams GN, Scoville CR, et al. Persistent disability associated with ankle sprains: A prospective examination of an athletic population. Foot Ankle Int 1998;19(10):653-660.
5. Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the international ankle consortium. J Orthop Sports Phys Ther 2013;43(8):585-591.
6. Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports 2002;12(3):129-135.
7. Saltzman CL, Salamon ML, Blanchard GM, et al. Epidemiology of ankle arthritis: Report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J 2005;25:44-46.
8. Soboroff S, Pappius EM, Komaroff AL. Benefits, rsk, and cost of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop 1984;(183):160-168.
9. Knowles SB, Marshall SW, Miller T, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prev 2007;13(6):416-421.
10. Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med 2008;27(3):353-370.
11. Brown C. Foot clearance in walking and running in individuals with ankle instability. Am J Sports Med 2011;39(8):1769-1776.
12. Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med 2006;34(12):1970-1976.
13. Delahunt E, Monaghan K, Caulfield B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J Orthop Res 2006;24(10):1991-2000.
14. Drewes LK, McKeon PO, Paolini G, et al. Altered ankle kinematics and shank-rear-foot coupling in those with chronic ankle instability. J Sport Rehab 2009;18(3):375-388.
15. Drewes LK, McKeon PO, Kerrigan DC, Hertel J. Dorsiflexion deficit during jogging with chronic ankle instability. J Sci Med Sport 2009;12(6):685-687.
16. Monaghan K, Delahunt E, Caulfield B. Ankle function during gait in patients with chronic ankle instability compared to controls. Clin Biomech 2006;21(2):168-174.
17. Morrison KE, Hudson DJ, Davis IS, et al. Plantar pressure during running in subjects with chronic ankle instability. Foot Ank Int 2010;31(11):994-1000.
18. Feger M, Donovan L, Hart J, Hertel J. Lower extremity muscle activation in patients with and without chronic ankle instability. J Athl Train [In Press]
19. Feger MA, Donovan L, Hart JM, Hertel J. Lower extremity muscle activation during functional exercises in patients with and without chronic ankle instability. PM R 2014 January 8. [Epub ahead of print]
20. Hertel J, Olmsted-Kramer LC. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture 2007;25(1):33-39.
21. McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: Can deficits be detected with instrumented testing? J Athl Train 2008;43(3):293-304.
22. McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord 2008;9(1):76.
23. Gribble PA, Hertel J, Denegar CR, Buckley WE. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train 2004;39(4):321-329.
24. Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train 2009;44(4):350-355.
25. Gribble PA, Kelly SE, Refshauge KM, Hiller CE. Interrater reliability of the star excursion balance test. J Athl Train 2013;48(5):621-626.
26. Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the star excursion in balance tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train 2002;37(4):501-506.
27. Gribble P, Robinson R. Differences in spatiotemporal landing variables during a dynamic stability task in subjects with CAI. Scand J Med Sci Sports 2010;20(1):1-9.
28. Loudon JK, Santos MJ, Franks L, Liu W. The effectiveness of active exercise as an intervention for functional ankle instability. Sports Med 2008;38(7):553-563.
29. Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med 1988;9(2):141-144.
30. Ross SE, Guskiewicz KM. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin J Sport Med 2006;16(4):323-328.
31. Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther 2007;37(6):303-311.
32. McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part II: Is balance training clinically effective? J Athl Train 2008;43(3):305-315.
33. Bahr R, Lian Ø, Bahr I. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: A prospective cohort study. Scand J Med Sci Sports 1997;7(3):172-177.
34. McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med 2006;34(7):1103-1111.
35. Verhagen E, van der Beek A, Twisk J, et al. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: A prospective controlled trial. Am J Sports Med 2004;32(6):1385-1393.
36. McKeon PO, Paolini G, Ingersoll CD, et al. Effects of balance training on gait parameters in patients with chronic ankle instability: A randomized controlled trial. Clin Rehabil 2009;23(7):609-621.
37. McKeon P, Ingersoll C, Kerrigan DC, et al. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc 2008;40(10):1810-1819.
38. O’Driscoll J, Kerin F, Delahunt E. Effect of a 6-week dynamic neuromuscular training programme on ankle joint function: A case report. Sports Med Arthrosc Rehabil Ther Technol 2011;3(1):13-19.
39. Donovan L, Hertel J. A new paradigm for rehabilitation of patients with chronic ankle instability. Phys Sportsmed 2012;40(4):41-51.











